Physical activity and recreational and competitive sports are not only an important part of our culture and leisure activities, but they also prevent many diseases. Exercise is also an effective treatment for at least 26 major diseases. However, COVID-19 mitigation measures have changed and often reduced physical activity. For example, Canadian and UK citizens were 30% to 40% less physically active, impacting physical and mental health.
Indoor group exercise in small, poorly ventilated rooms promotes SARS-CoV-2 infection.
SARS-CoV-2 and other airborne pathogens are transmitted via aerosol particles with a diameter of a few hundred micrometers and droplets of a few hundred micrometers or larger. Larger droplets carry pathogens during infections that occur when two people are up to ~1.5 m away from each other and quickly fall to the ground. In contrast, small aerosol particles float in the air, can carry pathogens such as SARS-CoV-2, and can mediate airborne infections.
Direct contact between people or through shared objects can also cause infections, but this is less likely. Several studies have shown that the concentration of aerosol particles in exhaled air varies greatly in the population. For example, approximately 20% of people emit more than 156 particles per liter of exhaled air. These individuals have been called “super emitters” . The number of aerosol particles emitted by a person per unit of time varies and increases when that person talks, coughs, sings, or is physically active.
It has also been shown that the number of aerosol particles emitted is influenced by the hydration status of the airways. Airway dehydration can be caused by exercise and increased ventilation and both can lead to a greater number of aerosol particles emitted. During exercise, ventilation (i.e., the air inhaled and exhaled by a person) increases from ~5 to 15 liters/min at rest to more than 100 liters/min in untrained individuals and can reach 200 liters/min in highly trained rowers .
Finally, people mildly infected with SARS-CoV-2 are reported to exhale a greater number of aerosol particles than uninfected people. Taken together, this suggests that people infected with SARS-CoV-2 who exercise will "expel" more SARS-CoV-2 into a room and that uninfected people who exercise will inhale more aerosol particles contaminated with SARS-CoV-2. 2, compared to resting.
Aerosol particle emission increases exponentially above moderate exercise intensity, resulting in super-emission during maximal exercise
Meaning
Airborne transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or other pathogens likely increases during indoor exercise , but data on the emission of aerosol particles by an exercising individual are lacking. Here, we report that aerosol particle emission increases on average 132-fold from 580 ± 489 particles/min at rest to 76,200 ± 48,000 particles/min during maximal exercise. Aerosol particle emission increases moderately up to an exercise intensity of ≈2 W/kg and exponentially at higher exercise intensities.
These data not only explain SARS-CoV-2 transmissions during indoor group exercise, but can also be used to design better targeted mitigation measures for indoor physical activity, such as physical education at school, dance events during weddings or high-intensity gym classes like spinning.
Summary
Many airborne pathogens, such as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), are transmitted indoors via aerosol particles. During exercise, lung ventilation can increase more than 10 times and therefore athletes exhale a greater volume of air containing aerosols.
However, we currently do not know how exercise affects the concentration of aerosol particles in exhaled air and the overall emission of aerosol particles. Accordingly, we developed a method to measure in parallel aerosol particle concentration in expired air, pulmonary ventilation, and aerosol particle emission at rest and during a graded stress test to exhaustion.
We used this method to evaluate eight women and eight men in a descriptive study. We found that the concentration of aerosol particles in expired air increased significantly from 56 ± 53 particles/liter at rest to 633 ± 422 particles/liter at maximum intensity.
Aerosol particle emission per subject increased significantly by a factor of 132 from 580 ± 489 particles/min at rest to a super emission of 76,200 ± 48,000 particles/min during maximal exercise.
There were no sex differences in aerosol particle emission, but resistance-trained subjects emitted significantly more aerosol particles during maximal exercise than untrained subjects. Overall, aerosol particle emission increased moderately up to an exercise intensity of ~2 W/kg and exponentially thereafter.
Together, these data could partly explain superspreading events , especially during high-intensity indoor group exercise, and suggest that strong infection prevention measures are needed , especially during exercise at an intensity exceeding ~2 W/kg . Investigations are needed into factors that influence aerosol particle generation, such as respiratory tract and whole-body hydration status during exercise.
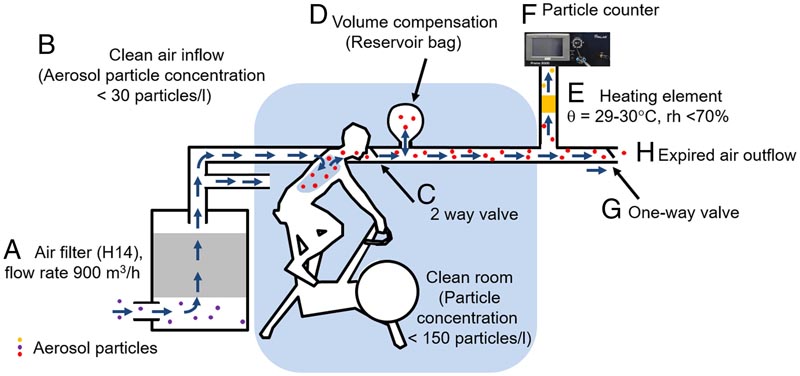
Schematic illustration of the experimental setup designed to measure ventilation, aerosol particle concentration, and aerosol particle emission over a wide range of ventilation, from rest to maximal exercise. The ambient air (A) was first filtered to generate air almost free of aerosol particles. The subject then inhaled the (B) clean air filtered through a silicone face mask covering the mouth and nose (not shown). The silicone mask was (C) connected to a two-way valve so that only exhaled air entered the outflow. A plastic bag acted as a buffer/reservoir (D). A pump diverted ~5 liters/min of exhaled air through first (E) a heated tube to remove condensation and then into (F) the Palas Promo 3000 particle counter. This counter uses a Welas 2300 sensor for particle detection. . The remaining air was released to the environment through a separate tube and one-way valve (G) so that ambient air could not enter the system. The experiment was conducted in a clean room to further reduce the risk of contamination by aerosol particles.
Discussion
The first main result of this descriptive study is that aerosol particle emission increases on average 132-fold from 580 ± 489 particles/min at rest to a super-emission of 76,200 ± 48,000 particles/min during maximal exercise in women and men healthy young people.
We also found that aerosol particle emission increases moderately up to an exercise intensity of ~2 W/kg and exponentially at higher exercise intensities.
This finding can be used to design better mitigation strategies for indoor group exercise. Third, aerosol particle emission at rest is only moderately correlated with aerosol particle emission during exercise.
We found that mean aerosol particle emission increased 132-fold from rest to maximal exercise.
We found that endurance-trained athletes emitted 85% more particles during maximal exercise than untrained subjects (P=0.02). This is intuitive since resistance-trained individuals also ventilate more aerosol-containing air into a room during maximal exercise.
In this study, resistance-trained subjects ventilated on average 25% more than untrained subjects during maximal exercise which was not significant due to large interindividual variation. This difference only partially explains the variation in particle emission between untrained subjects and resistance-trained subjects. The other factors contributing to the 85% difference in aerosol emission between trained and untrained subjects are unknown.
In summary , we report that aerosol particle emission increased by a factor of 132 from rest to maximal exercise with no significant differences between women and men, but between untrained and resistance-trained subjects during maximal exercise. Aerosol particle emission increases moderately up to an exercise intensity of 2 W/kg and exponentially at higher exercise intensities. This information should be used to develop further data-driven mitigation measures for indoor group exercise. |
















