Aerosols exist. Denying its existence is like denying rain.
An aerosol is defined as a particle (solid or liquid) that can remain suspended in the air (at least for “seconds”) and that is dispersed with air currents¹. The best-known aerosols are particles, PM for its acronym in English “particulate material” , suspended in the pollution of large cities. The aerosols under discussion today are those attributed to viral airborne transmission.
An adequate understanding of the viral transmission route and its interrelation with environmental pollution aerosols could explain and give rise to a hypothesis that justifies the lack of control in this pandemic.
Update on viral transmission routes:
In a recent classification of SARS2 COVID19 transmission, Dr. Donald Milton² (University of Maryland, USA), describes that there would be three routes of contagion:
1. The “fomite” route , also called passive vector or “surface contact” , fomite is a lifeless object, but with the properties of transmitting the disease (any germ); like a light switch, door handle, sheets…. and that after being in contact, contagion occurs by touching the mouth, nostrils or eyes.
2. The “big drop” or the “ballistic drop” . Droplets are particles of saliva or respiratory fluid (> 100 microns, where 1 micron (μm) is one thousandth of 1 mm) that are expelled by infected people when coughing, sneezing and, to a lesser extent, speaking. They fly ballistically (like a projectile) at a distance of less than 2 meters. They are contagious upon impact in the mouth, nostrils or eyes. If they do not impact, it falls on any surface (ground).
3. The “aerosol” route . Aerosols are also particles, but of saliva or respiratory fluid (also called microdroplets), with the ability to be suspended in air and disperse with air currents, but with a diameter < 100 microns. They can be divided according to their size and their ability to penetrate the respiratory system (it is similar to the classification of particles of environmental pollutants, which classifies them according to the place where they impact the respiratory tract).
The smaller the size of the aerosol, the greater the ability to suspend it in the air (from seconds to hours), will be able to travel longer distances, and will be influenced by air currents or air recirculation. That is, smaller aerosols will remain longer, travel farther in the air and can impact different parts of the human respiratory tract.
The difference is that ballistic droplets infect by impact and aerosols infect by inhalation. In figure 1, Milton² explains the ballistic route (direct trajectory, short distance and with large microdroplets, and is represented in blue). And then the 3 models of aerosols are observed as routes of contagion (represented by the colors red, yellow and green, depending on the size):
1) Respirable aerosols <2.5 μm: defined as those aerosols/particles small enough to reach the respiratory bronchioles and alveoli (red color)
2) Thoracic aerosols <10 μm: are those larger particles (up to 10 -15 μm) capable of penetrating the trachea and large intrathoracic airways. (yellow color)
3) Inhalable aerosols or total suspended particles: they are the largest aerosols, <100 microns and can penetrate the upper respiratory tract (green color).
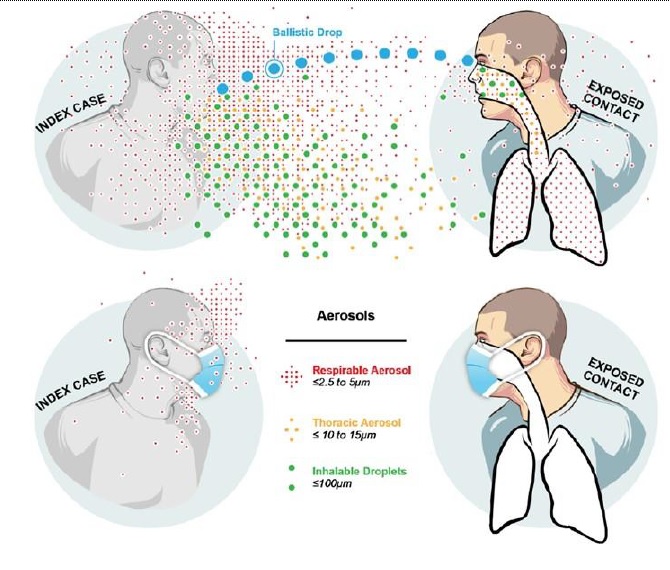
Figure 1: Schematic representation of droplet (blue) and aerosol (green, yellow, and red) infection pathways for a respiratory disease. Both travel through the air from the infected person to the susceptible person, but ballistic droplets infect by impact and aerosols infect by inhalation. (A Rosetta Stone for Understanding Infectious Drops and Aerosols. Donald K Milton. Journal of the Pediatric Infectious Diseases Society, Volume 9, Issue 4, 1 September 2020, Pages 413–415, https://doi.org/10.1093/jpids/ piaa079 Web: http://tinyurl.com/faqs-aerosol)
There is no doubt in the scientific literature about the existence of aerosols of various sizes, generated by exhalation, speaking, singing, coughing and sneezing, and which may be suspended in the air of a poorly or unventilated environment. Air is a gas that, even in closed places, is not still; it responds to the microclimate of the place and will be conditioned by temperature, pressure, humidity, among other physical variables. The same human body heat that we emit (especially in areas with greater numbers of people) can condition aerosols to flow on “warm rising currents”².
The coronavirus has an approximate diameter of 0.12 microns and is not floating in isolation in the air. They are immersed in and transported by these microdroplets/aerosols of variable size. There is also no doubt that COVID-19 viral material exists in these aerosols, and even replicable (which suggests viability).
This finding has been demonstrated in areas with high risk of aerosolization such as health centers³. And usually the highest concentration is found near or in ventilation ducts, as well as in bathrooms, medical staff4, hallways of health centers with COVID-19 and even under the bed of COVID-19 patients where one of the flows of The ventilation is oriented in that direction.
The multiple scientific examples (published and scientifically proven) of infections in closed places, with artificial ventilation and air recirculation (super-infections), end up closing the potential idea that the aerosols emanating from COVID 19 patients in non-ventilated places are potentially infective to distances much greater than the classically described 2 meters.
Super contagions cannot be explained except by the aerosol route. In a couple of hours, a single individual infected 52 others with coronavirus during a choir rehearsal with 61 people in Sakgit (Washington, United States) 6. This is one of the best-documented episodes of mass coronavirus infection to date. date, according to the United States Center for Disease Control (CDC). There is no way to explain it if it is not contagion through the aerosol route.
The episode of super contagion on a bus going to a religious ritual in China, or the case of the restaurant in Guangzhou (China)7, all multiple in places without ventilation and several meters away from patient zero, cannot be explained if it is not for the aerosol route. For some researchers, there is already enough scientific support to demonstrate that this would be the main route of transmission, accounting for 75% of total infections5.
It is important to note that, although we talk about “airborne transmission,” the chances of becoming infected in open spaces are 20 to 100 times lower than in closed spaces. Furthermore, the sun’s UV rays inactivate any virus in minutes, and the more airy the outdoor space is, the lower the chances of contagion.
On the other hand, there is no doubt about the importance of classic prevention measures. The meta-analysis published in the Lancet magazine “ Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis” , shows the importance physical distancing, face masks, and eye protection to prevent person-to-person transmission. However, in view of what is happening in our country and in the world, it does not seem to be enough.
The video of the simulation of aerosolization with and without a mask carried out by the Fugaku supercomputer (a petascale supercomputer developed by Fujitsu for the RIKEN Computer Science Center in Kobe, Japan, the fastest in the world with 7.5 million cores Figures 2 and 3), demonstrated at a glance how the mask prevents ballistic (direct) contamination, but does not completely inhibit aerosolization, with the N95 mask (used only in the medical field) being the most effective. That is to say, there would be a non-negligible percentage of aerosolization with conventional surgical oronasal masks and surely something more in homemade oronasal masks (misnamed tapabocas). Even more so... if they are not placed correctly.
The Fugaku supercomputer shows us filtration of very small aerosols, especially in the gaps where the fabric of the mask does not make contact with the skin (such as the nose/cheek angle). Therefore, masks are useful... but they are not enough. Prof. José Luis JImenez¹ compares exhaled tobacco smoke for practical and educational purposes to explain the concept of aerosol suspension in closed places. In fact, exhaled tobacco smoke is an aerosol type of environmental pollutant.
Individual bioprotection measures reduce contagion, but are not enough to abolish it, especially in high-risk places. It would then be necessary to inhibit the aerosolization of the place. In this portal we demonstrate the minimal contagion that the cabin staff had on the repatriated flights to Argentina with COVID 19, which occurred between March and April. I attribute this to the biosafety systems of the airplanes equipped with powerful high-efficiency HEPA 14 filters along with external air recirculation.
Today there are scientific works that refer to the biosafety elements of the airplane (Risk of COVID-19 During Air Travel, JAMA October 2020) 8. HEPA 14 filters filter 99.9% of viruses and other germs, and we proposed adapting the mechanism of filtering of airplanes and operating rooms in shops, closed spaces, offices, gyms, public transportation, universities, theaters, bars... etc¹5.
Now... What is the relationship between viral airborne aerosols and those from environmental pollution?
Aerosols from environmental pollution have been extensively studied. They are particulate matter (PM) in suspension that cause damage to our health (lung, heart and cancer). They consist of a complex mixture of solid and liquid particles of organic and inorganic substances suspended in the air. PM is one of the 4 environmental pollutants and affects more people than any other pollutant.
The main components of PM are nitrates, sulfates, mineral dusts, ammonia, sodium chloride, soot, and water. They are classically divided into PM < 10 microns and And this mortality is fundamentally due to chronic exposure to the smallest polluting aerosols: PM < 2.5 microns called “respirable particles.” The smaller the PM, the more likely they are to reach the deep lung (bronchioles and alveoli) with the potential to pass into the circulation (blood) by diffusion (alveolar-capillary exchange). And the greater the depth... the greater the damage.
This mechanism of damage due to environmental contamination of small particles (PM <2.5) has been widely demonstrated and introduces us to a hypothesis: if the “respirable” viral airborne aerosols (< 2.5 microns) also had the capacity to directly impact alveoli …would a more rapid and severe SARS-2 pneumonia then occur?
The inoculation of this coronavirus in the nasal passages has been widely demonstrated, and it is described as the main route of entry (above the pharynx and conjunctiva)... But is this access door the only direct entrance to the respiratory system? It could be that the largest aerosols and microdroplets impact the nasal passages and the medium ones in the upper respiratory tract and the smallest ones in the lower respiratory tract.
This is not a new hypothesis. Already in 1966, Dr. Robert Alford ¹¹ investigated the routes of contagion of the Influenza virus, comparing inhalation versus nasal instillation; and he suggested that with small aerosols the viral load required for contagion was lower but at the same time the severity was greater. That is, he described the anisotropic properties of a virus (the clinical response changes depending on the direction of the virus, size, place of inoculation, microclimate... etc). Dr. Donad Milton in 2012 in his review article “What was the primary mode of smallpox transmission?” Implications for biodefense” ¹¹ (“What was the main mode of transmission of smallpox? Implications for biodefense”) published in the prestigious journal “Cellular And Infection Microbiology”, describes a hypothetical scenario of bioterrorism due to Smallpox.
In this work he investigated the possible routes of transmission of smallpox as a prevention of a biological attack. In that article he postulated as probable the theory that, the smaller the size of the aerosols, there would be greater damage and even greater mortality. It says: “if smallpox can be transmitted via airborne microdroplets with aerodynamic diameters of ≤2.5 μm (microns) capable of remaining suspended in the air for hours and depositing in the lower part of the lung, then the systems of mechanically recirculated air would increase the contact rate, the R0, the risk of epidemic spread and the difficulty of controlling hospital infections. ” Any resemblance to reality is NOT mere coincidence.
The article also refers to the deeper the impact of small aerosols (<2.5 microns) in relation to the respiratory tree, the more severe the smallpox disease may be. Milton concludes in his article on variolation and bio-terrorism: “smallpox appears not to have been transmitted with the same efficiency and virulence by all routes, whether aerosol, large droplets, or direct contact and skin inoculation. It appears to have been transmitted more efficiently and virulently by fine particle aerosols… ”
That is, smallpox would also have anisotropic properties like the influenza virus. And will the SARS-2/COVID-19 coronavirus have anisotropic properties? That is to say... could the clinical response change depending on which part of the respiratory system it impacts?
Although the hypothesis may also be valid for this coronavirus, it is not so easy to prove it nor has it yet been proven. The cause why some individuals have greater symptoms and greater severity remains debated. In addition to the viral load, the exposure time, individual susceptibility (multi-origin), the history and the tenor of the inflammatory response; The argument that the transmission route of very small aerosols directly reaches the alveoli could be a hypothesis that explains the greater speed and severity of the disease.
On the other hand, face masks reduce aerosolization, but do not inhibit it completely. And its incorrect use is not uncommon. And COVID 19 patients who wear masks do not have them on properly all the time either. The reality is that it is very difficult to keep it on properly when we feel bad and short of breath. And it has already been demonstrated in health centers that COVID 19 viral genetic material exists in the air and on surfaces.
If when we exhale the aerosols from the masks that filter out are the smallest (the macrodroplets remain impacted on the mask)... Could it be explained why, even though the use of face masks is mandatory, some patients directly present with symptoms of pneumonia? As occurs in environmental contamination and was suggested in the transmission of smallpox, contaminated aerosols < 2.5 microns (the smallest and those that remain suspended the longest) could directly impact the lower part of the lung tree. Although there is no answer today, it is a hypothesis that requires consideration.
One of the options to reduce aerosol contagion in closed areas with a high risk of infection is electronic biosafety elements with high-efficiency filter systems (HEPA 14) combined with germicides (for example, a non-toxic UV light). that guarantee filtration of aerosols (of all sizes) and frequent exchange of ambient air. The few published examples where, in addition to personal protection elements, high-efficiency filters and positive pressure among other biosafety elements are incorporated, demonstrated up to a zero level of interpersonal contagion.
Something humanity underestimated so that in the 21st century there is no control nor is it known where the main mechanism of viral transmission of this coronavirus really is. The classic routes of viral transmission (incorporated without changes since 1930) are not enough to explain the scope of this pandemic. The comings and goings of an Institution like the WHO in recommending the use of masks in the community (and even in the medical community!) is a clear example. And this September 21, in an incredible oversight labeled “unforced error,” the prestigious US CDC eliminates what it confirms within 24 hours. It describes on its website¹² that given the evidence of aerosols as an important route of contagion in closed or poorly ventilated places, air purification systems based on filters and UV lamps could be useful.
After having been eliminated, a similar statement and with the same recommendations was issued 8 days later (September 29) by the International Air Quality and Health Laboratory of the Queensland University of Technology, Brisbane, Australia¹³, and for the same 293 prestigious scientists who urged the WHO to modify its assessment of the route of contagion of aerosols. Some of these researchers even advise the CDC. Clearly “politics has reasons that reason does not understand.”
For that reason and perhaps... in the underestimation of the aerosol transmission route in closed and poorly ventilated places, and in the hypothesis (not yet studied) of the anisotropic property of this virus, one of the causes of the origin of so much contagion may lie. .
Finally, I could list the ten rules of aerosolization in this way:
1- Aerosols exist.
2- Aerosol is any liquid or solid particle, with the ability to remain suspended in air, but easily dispersed with air currents.
3- Environmental pollution aerosols are particles of PM <10 microns and PM <2.5 microns in diameter whose inhalation damages our health. PM < 2.5 microns are the most dangerous because they reach deep into the respiratory tree and can cross the alveolar-capillary barrier.
4- In the route of contagion of a respiratory virus, the “ballistic” macrodroplet hits directly at a short distance and is easily inhibited by a mask. Everything else (except surface infection) is aerosol contagion. Therefore, today it would be the main route of contagion.
5- The aerosols that we eliminate when we cough, sneeze, speak loudly, sing... etc., are microdroplets that are less than 100 microns, and can be divided into 3 types of aerosols according to their size and according to their ability to penetrate the respiratory tree. . (< 2.5 microns, < 10 microns and < 100 microns)
6- Aerosols in risk areas (COVID19 patient) may have replicable viral material.
7- Data based on observation and tracking, rigorously evaluated and published in scientific journals and websites, demonstrate that in superinfections in closed places and with air recirculation, the only possible transmission route several meters away from patient zero is the aerosol route. .
8- The chances of contagion in outdoor space are 20 to 100 times less than in closed places. It will depend on sun, wind, humidity... and proximity (without a mask and at a short distance we still get infected)
9- Masks (medical and homemade) partially inhibit aerosolization. It depends on its correct use and the type of mask how effective it will be. They are useful, but they are not 100% effective. And they are very useful in direct contagion (macrogout)
10- High-efficiency filtering systems combined with germicides (such as non-toxic UV light) can be useful to reduce “in situ” (and with human presence) the aerosolization of a high-risk place. Ozone in night mode complements the disinfection of surface contagion (fomites).
Author: Dr. Martin Lombardero: Cardiologist, Head of Cardiac Imaging Sanatoriums of La Trinidad Palermo, San Isidro and Ramos Mejía. (CABA and Province of Bs. As., Argentina).















