Link to Crohn’s disease detected in ultra-processed foods
High consumption of ultra-processed foods increases the risk of developing Crohn’s disease, according to the results of a large meta-analysis, but not ulcerative colitis.
Background and objectives Several studies have been published on the association between food processing and the risks of Crohn’s disease (CD) and ulcerative colitis (UC), with some variability in the results. We conducted a systematic literature review and meta-analysis to study this association. Methods From PubMed, Medline, and Embase through October 2022, we identified cohort studies that studied the association between food processing and the risk of CD or UC. The risk of bias of the included studies was assessed using the Newcastle-Ottawa scale. We calculated pooled hazard ratios (HRs) and 95% confidence intervals (CIs) using a random-effects meta-analysis based on estimates and standard errors. Results A total of 1,068,425 participants (13,594,422 person-years) were included among 5 cohort studies published between 2020 and 2022. Four of the 5 included studies were rated as high quality . The average age of the participants ranged from 43 to 56 years; between 55% and 83% were women. During follow-up, 916 participants developed Crohn’s disease (CD) and 1934 developed ulcerative colitis (UC). There was an increased risk of developing CD in participants with a higher consumption of ultra-processed foods compared to those with a lower consumption (HR, 1.71; 95% CI, 1.37–2.14; I 2 = 0 %) and a lower risk of CHD for participants with higher consumption of unprocessed or minimally processed foods compared to those with lower consumption (HR, 0.71; 95% CI, 0.53–0. .94; I 2 = 11%). There was no association between UC risk and ultra-processed foods (HR, 1.17; 95% CI, 0.86–1.61; I 2 = 74%) or unprocessed/minimally processed foods ( HR, 0.84; 95% CI, 0.68–1.02; i2 = 0%). Conclusions Higher intake of ultra-processed foods and lower intake of unprocessed or minimally processed foods are associated with an increased risk of CD, but not UC. |

Comments
Ultra-processed foods contain large amounts of artificial flavorings, stabilizers, emulsifiers, sweeteners or preservatives. Studies have linked greater consumption of them with cardiovascular diseases, diabetes, obesity and cancer.
For their research, published in Clinical Gastroenterology and Hepatology , Neeraj Nerula, MD of McMaster University, Hamilton, Ontario, and colleagues combined data from five recent cohort studies to evaluate whether their consumption was also linked to inflammatory bowel disease.
Collectively, the included cohort studies recruited more than 1 million participants (mean age, 43-56; 55%-85% women). Of these, 916 developed Crohn’s disease and 1,934 developed ulcerative colitis during follow-up. None of the participants had IBD at baseline and all were followed for at least 1 year. All of the studies used the same food classification system, called NOVA, to evaluate foods consumed, and all were conducted between 2020 and 2022.
People who consumed more ultra-processed foods had a higher risk of Crohn’s disease, compared with those classified as consuming lower amounts of these foods (hazard ratio, 1.71; 95% confidence interval, 1.37). -2.14). Additionally, a lower risk of Crohn’s disease was seen among participants who consumed more unprocessed or minimally processed foods, such as vegetables, chicken, milk, and eggs (HR, 0.71; 95% CI, 0.53-0. 94). The same associations were not observed for ulcerative colitis.
"Our findings support the hypothesis that consumption of [ultra-processed foods] and low consumption of unprocessed or minimally processed foods may increase the risk of CHD," Dr. Nerula and colleagues wrote. The lack of association observed with ulcerative colitis could be explained by differences in the pathogenesis of each disease.
Ultra-processed foods could contribute to Crohn’s disease by altering the gut microbiota , the authors wrote. “For example, emulsifiers have been shown to increase epithelial permeability, intestinal barrier disruption, and intestinal dysbiosis in mice. Carboxymethylcellulose has been shown to facilitate bacterial adherence to the intestinal epithelium, possibly leading to bacterial overgrowth and invasion of bacteria between the intestinal villi. Additionally, additives such as carrageenan, titanium dioxide, and maltodextrin have been shown to promote intestinal inflammation.”
Dr. Nerula and colleagues described the large size, low heterogeneity of the included studies, and the use of standardized, validated questionnaires to measure dietary intake in each study as strengths of their study. However, they cautioned that the results might not apply to younger age groups, and most of the participants were white Americans and Europeans, making the results difficult to generalize.
"Advances in food processing and associated changes in dietary patterns could explain the increased incidence of IBD during the 20th and 21st centuries," Dr. Narula and colleagues concluded. "Further research is needed to identify specific potential culprits among processed foods that could explain the observed increased CHD risk."
The study authors did not report external funding. Dr. Narula disclosed receiving fees from pharmaceutical manufacturers, including Janssen, AbbVie, Takeda, Pfizer, Merck and others. Two of the co-authors also disclosed receipt of industry funding, and five additional co-authors had no conflicts.
Ultra-processed foods and risk of Crohn’s disease: how much is too much?
Associations of micro/macronutrients and, more recently, whole diet quality scores, with the development of inflammatory bowel disease in large prospective longitudinal studies have yielded inconsistent results with some degree of ambiguity. The interesting new development is the consistency of an association between the intake of ultra-processed foods (UPF) and the development of Crohn’s disease (CD), but not ulcerative colitis (UC), in disparate cohorts, as described convincingly in the meta-analysis of more than a million people worldwide by Narula and colleagues.
CD is thus added to the list of non-communicable diseases associated with ultra-processed foods (UPF), which include mortality from all causes, cancer, cardiovascular diseases and obesity.
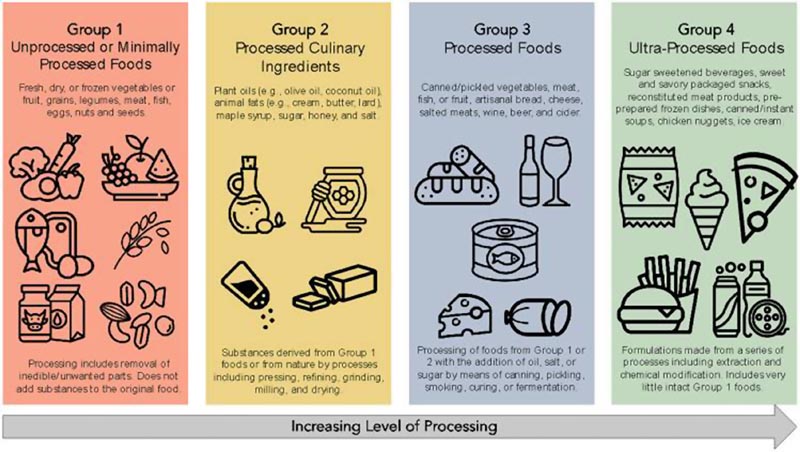
UPFs are defined according to the NOVA classification system (Figure) which has been widely used for retrospective assessments of UPF intake from food frequency questionnaires, associating UPF as a proportion of dietary intake with the development of diseases. over decades of high-quality prospective cohort studies. Narula et al reported that the highest quartile of UPF intake had a higher risk of developing CD (pooled hazard ratio [HR], 1.71; 95% confidence interval [CI], 1.37–2.14). compared to the lowest quartile of intake.
In contrast, higher intake of unprocessed foods decreased the risk of CHD (pooled HR, 0.71; 95% CI, 0.53–0.94). It is important to note that these relationships were not significant for UC.