In December 2019, a cluster of severe respiratory infections was reported in Wuhan, Hubei Province, China. In January 2020, the first case of death from the virus was reported in China. Reports of positive cases from other countries such as Thailand, Japan, South Korea and the US have made matters worse. The result of this major epidemic is the filling of hospital beds, excessive fatigue of the medical team, serious lack of personal protective equipment, infection of hospital staff, lack of manpower and the spread of diseases and the anxiety of people in countries around the world.
Numerous evidences show that COVID-19 can affect different organs of the human body as part of ’long COVID-19’ such as Guillain-Barré syndrome, pulmonary fibrosis, pulmonary embolism, cardiomyopathy, skin and joints, sensory dysfunction and stroke.
’Long COVID-19’ is a term used to describe symptoms in patients that continue for weeks or months after recovery from COVID-19.
Some cadaveric studies confirm the presence of intravascular thrombosis and coagulopathy in patients with COVID-19 infection, which may be one of the causes of avascular necrosis of the femoral head in these patients. Numerous cases have been reported with a diagnosis of avascular necrosis or reactive arthritis after COVID-19 infection. All of these patients were treated with one dose of corticosteroids (CS) as part of the COVID-19 treatment regimen.
To date, no cases of purulent joint infection due to COVID-19 infection have been reported, and in particular the association of septic arthritis with avascular necrosis has not been reported. In this article, we report five cases with septic arthritis of the hip joints with some degree of AVN of the femoral head after recovery from COVID-19 disease.
All of them received CS (methylprednisolone, prednisolone, dexamethasone) during the COVID-19 disease period along with other antiviral medications. All of these cases were negative for antinuclear antibodies, rheumatoid factor, anti-cyclic citrullinated peptide antibodies, hepatitis B virus surface antigen, anti-hepatitis C virus antibodies, and anti-human immunodeficiency virus antibodies. Examination of the joint fluid for crystals was also negative in all cases.
Aim
At present, concomitant avascular necrosis (AVN) of the femoral head and septic arthritis (SA) as a sequel to COVID-19 infection have not yet been documented. Through the large-scale use of life-saving corticosteroids (CS) in COVID-19 cases, we aim to warn against the occurrence of hip joint infection in these patients.
Methods
We present a series of five cases in which patients developed septic arthritis concomitant with avascular necrosis (AVN) after being treated for COVID-19 infection.
The mean dose of prednisolone used in these cases was 1,695.2 mg. The time of onset of hip symptoms in our cases from the onset of COVID-19 infection was 56 days in the first case, 43 days in the second case, 30 days in the third case, 29 days in the fourth case and 50 days days in the last case, with an average time of 41.6 days .
All patients underwent surgery depending on the extent of articular cartilage damage using a direct anterior approach.
Results
Clinical and laboratory symptoms improved significantly in all patients. The patients’ mean visual analogue pain score decreased from 9.4 (9-10) before surgery to 2.8 (1-4) after 1 week of operation.
Imaging findings
Preoperative imaging was performed for all patients, including a standard pelvic radiograph (anteroposterior view) and also a pelvic and hip MRI with a standard protocol. MRI with gadolinium was performed in two cases (case two and case four).
X-ray evaluation shows sclerosis and collapse of the femoral head consistent with classic avascular necrosis. An X-ray clue for the presence of an intra-articular inflammatory process was displaced gluteal fat planes . Narrowing of the joint space was observed in cases with cartilage damage.
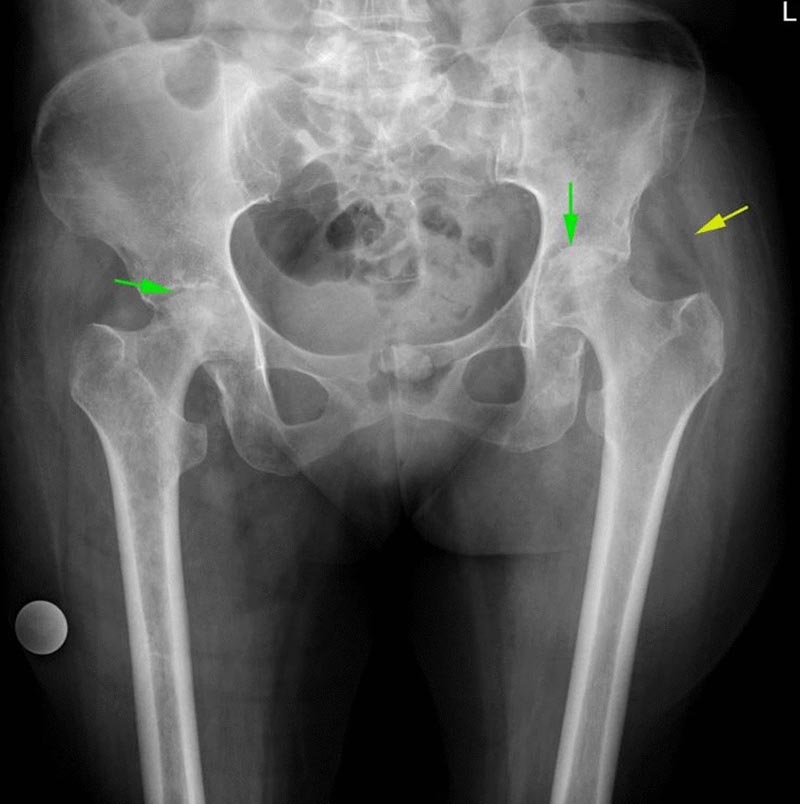
AP view of the pelvic radiograph shows sclerosis and collapse of the bilateral femoral head in favor of the AVN femoral head (green arrow). Soft tissue edema and displaced gluteal fat planes are in favor of joint fluid and possible inflammatory process (Yellow arrow)
On MRI evaluation , all patients show classic AVN findings of the femoral head such as bone marrow edema and serpiginous lines of abnormal signal on the superior and medial aspect of the femoral head.
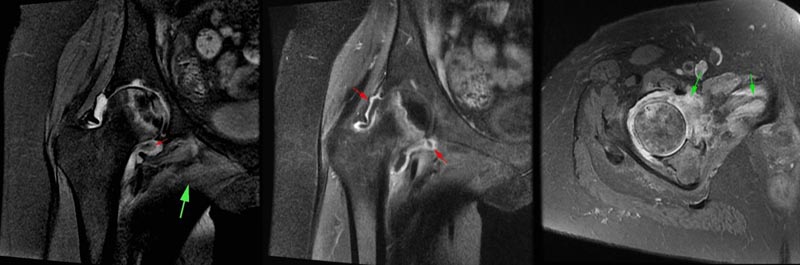
a Coronal PD fat satellite images show femoral AVN in association with joint effusion and synovial thickening (small red arrow). There is also edema in the adductor muscle group (large green arrow). b Coronal T1 satellite images in the same patient as (a) showing synovial thickening and enhancement after contrast injection (red arrow). c Axial oblique satellite images of PD in another patient showing edema in the pectineus muscle and also in the inferior capsule of the hip joint (green arrow).
An additional finding was the presence of joint effusion in the affected hip joint. Mild reactive effusion could be observed in association with AVN of the femoral head, especially in the advanced stage due to superimposed degenerative changes.
In the cases included in our study, the amount of joint effusion was greater than expected and was associated with synovial thickening and enhancement. An important clue was edema and inflammation in the periarticular soft tissue, including the adductor and gluteal muscle groups, which were not routinely observed in AVN of the femoral head.
In cases with prolonged symptoms (all cases), cartilage damage and superimposed degenerative changes developed.
Conclusions In any patient with a history of COVID-19 infection, especially those who have been treated with corticosteroids as one of the medications prescribed during the illness, any joint symptoms, especially in the hips, should draw our attention to the joint infection, and with Timely diagnosis and surgery, the hip joint can be saved. |
Discussion
Joint symptoms have been observed in several patients with COVID-19 infection during the recent pandemic event. These joint disorders can have different etiologies and occur in different joints. For example, medications used to treat the infectious disease COVID-19, such as CS, can have side effects on the hip joints and several cases of AVN in the femoral head have been reported after treatment of the COVID-19 disease. in people treated with CS.
These reports indicate that the occurrence of AVN of the femoral head in patients with COVID-19 was associated with lower doses and shorter duration of CS administration compared to other patients with avascular necrosis of the femoral head who did not have disease. by COVID-19. Furthermore, endothelial markers were found to be elevated in the blood of critically ill COVID-19 patients.
Utoppsy of many of these patients confirmed endothelial dysfunction. This endothelial destruction can trigger proinflammatory and procoagulant pathways and can lead to widespread microcirculatory dysfunction and related microthrombi that could be one of the causes of avascular necrosis of the femoral head in patients with COVID-19 infection.
Reactive arthritis is another form of joint complication caused by different types of infections, which can be related to mucosal infections in different areas of the body, such as urogenital (chlamydia) and gastrointestinal (campylobacter, salmonella, shigella, clostridium difficile, Yersinia) and respiratory pathogens (chlamydia pneumonia). Its incidence is reported to be 1 to 1.5% in gastrointestinal infections and 4 to 8% after urogenital tract infections.
People with the HLA-B27 allele or a family history of spondyloarthropathies are at greater risk of developing reactive arthritis. Most cases of this type of arthritis are seen in the lower extremities and this is considered a major diagnostic criterion for the diagnosis of reactive arthritis. The prognosis is favorable in most cases and spontaneous improvement is seen in most cases within 6 to 12 months.
Recently, cases of reactive arthritis associated with COVID-19 disease have been reported in lower limbs such as knees, ankles, metatarsophalangeal and interphalangeal joints. One case of reactive arthritis following COVID-19 disease in the wrist and shoulder has also been reported.
The most appropriate treatment for septic arthritis is joint drainage and administration of appropriate antibiotics based on culture and antibiogram results. Complete removal of necrotic and infectious material is mandatory. Joint drainage methods include closed drainage, arthroscopic drainage, and open drainage, especially in the hip joints.
The suitability and appropriateness of antibiotic type , dose and duration are determined in the literature and should cover the most common pathogens (staphylococcus aureus and streptococcus).
In patients with a history of recent intensive care unit hospitalization and other risk factors for MRSA, the antibiotic regimen should consist of vancomycin with or without second or third generation cephalosporin and in patients at high risk of gram-negative sepsis (elderly, UTI , catheters) should include second and third generation cephalosporins with or without fluoroquinolones . Consultation with an infectious disease specialist is strongly recommended.
To the best of our knowledge, this study reports the first cases of septic arthritis in the field of COVID-19 infection and its treatment and given the current pandemic we expect more in the future.
In any patient with a history of COVID-19 infection, especially those who have been treated with corticosteroids as one of the medications prescribed during the illness, any joint symptoms, especially in the hips, should draw our attention to the joint infection and take appropriate measures. necessary measures in this regard.