Compiled reports of acute hepatitis incidence and adenovirus isolation rates in children over the past year compared to a pre-COVID baseline showed no increase in the likelihood of either event.
In a recent small outbreak of acute childhood hepatitis of unknown etiology within a US healthcare system, many (but not all) of the patients tested positive for adenovirus type 40/41 (a virus that commonly resides in the large intestine of young children), suggesting that the two simultaneous findings could represent an etiological link.
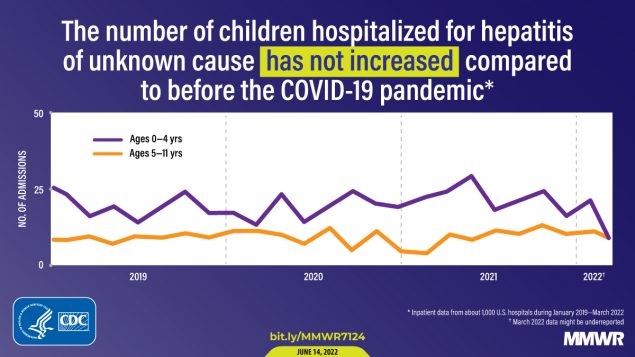
Now, CDC has presented data from several reports of hospitalizations or emergency department visits associated with pediatric hepatitis, liver transplant, and adenovirus 40/41 isolation during two periods: October 2021 to March 2022 and January 2018 as of February 2020 (i.e., pre-COVID-19 baseline). The two comparative periods were chosen based on the theory that healthcare seeking for this age group may have increased during the COVID-19 era.
The data did not show an increase in acute childhood hepatitis or an increase in adenovirus 40/41 isolation.
The initial report of childhood hepatitis and adenovirus isolation did not prove an etiologic link between the two findings. Current data, which show no increase in either hepatitis or adenovirus 40/41, do not disprove this possible connection. To date, neither hepatitis of unknown etiology nor the isolation of adenovirus 40/41 have constituted reportable findings. Resolving an etiological relationship will require, at a minimum, diligent reporting of both events.
What is known about this topic?
Following the identification of cases of pediatric hepatitis of unknown etiology in the United States and the United Kingdom, CDC issued a request in April 2022 for US providers to report additional cases. Many reported cases tested positive for adenovirus, which is not known to cause hepatitis in immunocompetent children.
What does this report add?
Analyzes of four data sources indicated no recent increases in emergency department visits or hospitalizations associated with hepatitis, liver transplants, or adenovirus types 40/41 percent positivity among U.S. children compared to pre-AIDS levels COVID-19 pandemic.
What are the implications for public health practice?
Current data do not suggest an increase in pediatric hepatitis or adenovirus types 40/41 above pre-COVID-19 pandemic baseline levels; Continuous monitoring is important to monitor changes over time.
These analyses, based on four data sources, did not indicate a recent increase in hospitalizations or emergency room visits associated with hepatitis among children aged 0 to 11 years, liver transplants among children aged 0 to 17 years, or the percentage of samples positive for adenovirus types 40/41 among children aged 0 to 9 years in the United States compared to pre-COVID-19 pandemic levels.
The potential role of adenovirus in the etiology of recently reported hepatitis cases is unknown; Ongoing research is evaluating this hypothesis along with the possible role of other factors, including current or past infections with SARS-CoV-2, the virus that causes COVID-19.
It is still unknown whether the recently reported cases represent a new etiology of pediatric acute hepatitis or a previously existing phenomenon that is now being detected.
The rarity of this result makes it difficult to detect small changes, and pandemic-associated disruptions in health care-seeking behavior and infectious disease epidemiology could still be normalizing. Continued assessment of trends, in addition to improved epidemiologic investigations, will help contextualize reported cases of acute hepatitis of unknown etiology in American children.
















