Key points What are the linear and nonlinear associations between various sex-specific risk factors and the occurrence of atrial fibrillation (AF) in women? Findings In this cohort study of 235,191 women without AF at baseline, a history of early or late menopause or irregular menstrual cycles was significantly associated with an increased risk of new-onset AF. Both nulliparity and multiparity were also significantly associated with an increased risk of AF. Meaning The findings of this study suggest that AF screening and prevention strategies should take into account women’s reproductive history. |
Atrial fibrillation (AF) is the most common cardiac arrhythmia worldwide and carries a high risk of morbidity and mortality. Evidence suggests differences in the pathophysiological processes of AF between men and women and an association of AF with a poor prognosis among women. These findings warrant further investigation into sex-specific risk factors in the development of AF.
Sex hormones may play a key role in cardiovascular health. The suggested benefits of estrogen for cholesterol metabolism and endothelial function decrease as a woman ages. This age-related decline in estrogen levels, particularly after menopause, has been associated with an increased risk of cardiovascular disease (CVD).5
It is known that the pathophysiological processes of AF are complex and multifaceted. An electrophysiological dysfunction within the heart, including an altered refractory period and action potential duration, is thought to be one of the most important factors in the onset of AF. Despite the lack of direct evidence, estrogens may confer an advantage in AF by extending atrial conduction time, action potential duration, and effective atrial refractory period. Therefore, we speculate that reproductive lifespan function is potentially associated with the development of AF in women, induced by long-lasting changes in estrogen levels related to aging.
Although associations of menopausal age and reproductive lifespan with incident AF have been reported, a comprehensive evaluation of the possible association of a wide range of reproductive lifespan factors with the development of AF is scarce. In the present study, we aimed to investigate potential linear and non-linear associations between sex-specific risk factors and the risk of new-onset atrial fibrillation among a large population of women in the UK Biobank study.
Summary
Importance
Atrial fibrillation (AF) is the most common cardiac arrhythmia worldwide, with different epidemiological and pathophysiological processes for women vs. men and a worse prognosis for women. Further investigation of sex-specific risk factors associated with the development of AF in women is warranted.
Aim
To investigate potential linear and nonlinear associations between sex-specific risk factors and the risk of new-onset atrial fibrillation in women.
Design, environment and participants
This population-based cohort study derived data from the UK Biobank study from 2006 to 2010, a cohort of over 500,000 participants aged 40 to 69 years. Participants were women without atrial fibrillation and a history of hysterectomy or bilateral oophorectomy at baseline. The median follow-up period for AF onset was 11.6 years and follow-up ended on October 3, 2020.
Exhibitions
Self-reported sex-specific risk factors, including age at menarche, history of irregular menstrual cycle, menopausal status, age at menopause, years after menopause, age at first live birth, years after last birth, history of spontaneous abortions, history of stillbirths, number of live births and total reproductive years.
Main results and measures
The primary outcome was new-onset AF, which was defined using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision code I48.
Results
A total of 235,191 women (mean [SD] age, 55.7 [8.1] years) were included in the present study. During follow-up, 4629 (2.0%) women experienced new-onset AF.
In multivariable-adjusted models, a history of irregular menstrual cycle was associated with an increased risk of atrial fibrillation (hazard ratio [HR], 1.34; 95% CI, 1.01-1.79).
Both early menarche (age 7-11 years; HR, 1.10 [95% CI, 1.00-1.21]) and late menarche (age 13-18 years; HR, 1.08 [95% CI, 1.00-1.21]) , 1.00-1.17]) were associated with AF incidence. Early menopause (age 35-44 years; HR, 1.24 [95% CI, 1.10-1.39]) and late menopause (age ≥60 years; HR, 1.34 [95% CI, 1 .10-1.78]) were associated with a higher risk of PA.
Compared with women with 1 or 2 live births, those with 0 live births (HR, 1.13; 95% CI, 1.04-1.24) or 7 or more live births (HR, 1.67; 95% CI, 1.03-2.70) both had a significantly higher risk of AF.
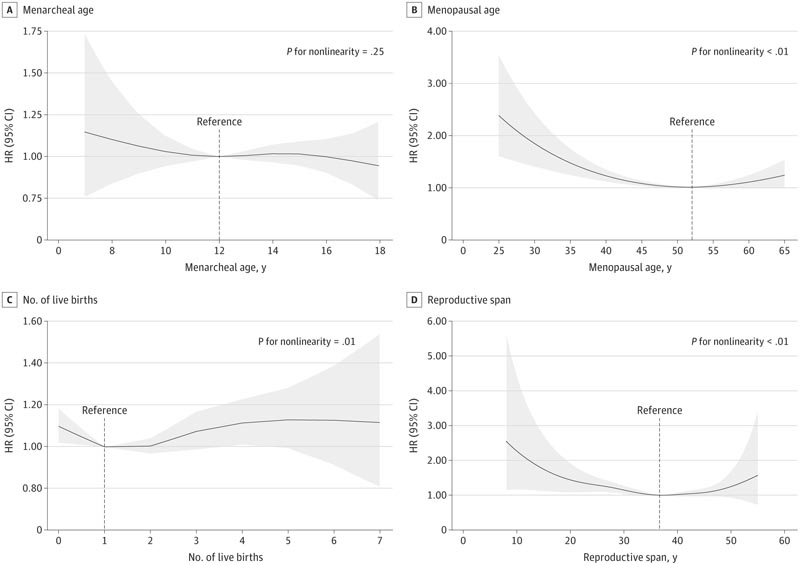
Figure : Nonlinear association between sex-specific risk factors and risk of new-onset atrial fibrillation. The model was adjusted for baseline age, race and ethnicity, educational level, body mass index, total cholesterol, high-density lipoprotein cholesterol, systolic blood pressure, diastolic blood pressure, smoking, history of diabetes, history of coronary heart disease, history of heart failure, history of stroke, use of blood pressure-lowering medications, and use of cholesterol-lowering medications. Shaded areas indicate 95% CIs. HR indicates the risk ratio.
Conclusions and relevance
The results of this study suggest that irregular menstrual cycles, nulliparity, and multiparity were associated with an increased risk of new-onset atrial fibrillation among women. The results highlight the importance of considering women’s reproductive history when designing screening strategies for AF prevention.
















