Thrombocytopenia is defined as a platelet count of < 150 × 10 9 /L and occurs frequently in critically ill patients.
The condition arises as a result of reduced production or increased destruction or consumption of platelets.
Thrombocytopenia in critically ill patients is often a consequence of multiple pathophysiological mechanisms. These must be identified if the prognosis is to be determined and appropriate treatment provided.
This article provides an overview of thrombocytopenia in critically ill patients, including its pathophysiological mechanisms, course, evaluation, and treatment. The work is based on literature identified through a non-systematic search of the PubMed database and the authors’ own clinical experience.
| Prevalence and definition |
In a recent clinical study of patients in intensive care and observation units, thrombocytopenia was defined as mild (100-149 × 10 9 /L), moderate (51-99 × 10 9 /L), or severe (<50 × 10 9 /L), with reported incidences of 15.3%, 5.1% and 1.6%, respectively. The incidence of new-onset thrombocytopenia among intensive care patients ranges from 14% to 44%. More than half of those who spend more than two weeks in intensive care develop thrombocytopenia, which is associated with high mortality.
| Pathophysiological mechanisms |
Platelets are produced in the bone marrow from megakaryocytes, have a lifespan of 8 to 10 days, and are destroyed primarily in the spleen. They are essential for hemostasis and also contribute to angiogenesis and innate immunity.
The causes of thrombocytopenia can be divided into three main categories: reduced production, increased destruction, and increased consumption of platelets. A single patient can often exhibit more than one of these pathophysiological mechanisms simultaneously ( Figure 1 ). Platelet dysfunction is relatively common in critically ill patients and may be due to uremia, liver failure, or the use of medications or a heart-lung machine.
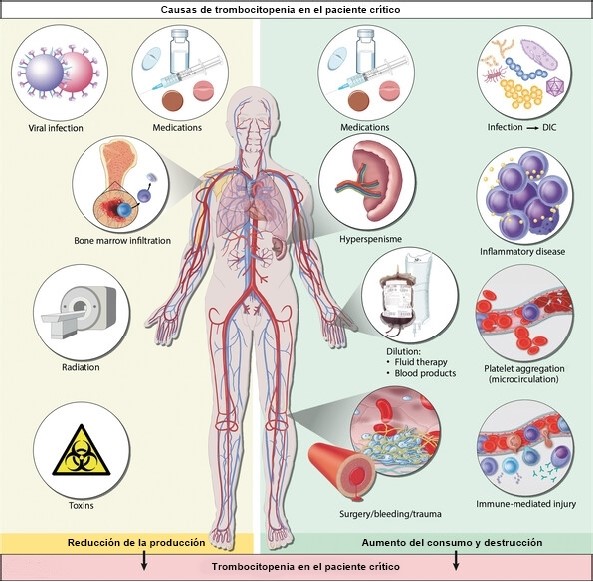
Figure 1. Thrombocytopenia is common in critically ill patients and is often the result of several different pathophysiological mechanisms. The causes can be divided into three main categories: reduced platelet production (bone marrow disease, use of chemotherapy or radiotherapy, acute and chronic viral infections, and poisonings); increased platelet consumption (physiological platelet activation during surgery/trauma/bleeding, pathological platelet activation such as in cases of disseminated intravascular coagulation (DIC), which is most often triggered by severe infection/sepsis) and increased platelet destruction ( hypersplenism, immunologically mediated drug hypersensitivity reactions and autoantibody formation, inflammatory diseases, such as hemophagocytic lymphohistiocytosis, and platelet aggregation in the microcirculation, as in cases of thrombotic microangiopathy). Additionally, thrombocytopenia may occur as a result of a dilution effect following massive transfusion of fluids or blood products.
> Production reduction
It is unclear to what extent reduced platelet production contributes to thrombocytopenia in critically ill patients. Individuals who have undergone cytotoxic chemotherapy show reduced production, as do those with bone marrow disease or acute alcohol toxicity. Both acute and chronic viral infections, including hepatitis C, cytomegalovirus, Epstein-Barr virus, and parvovirus B19, can inhibit platelet production. Thrombocytopenia has also been described in patients with severe COVID-19.
> Increase in consumption
Platelets can be activated by leukocytes, the complement system, coagulation factors, microorganisms, and tissue damage. They also play a key role in the immune response. Thrombin-mediated platelet activation may be physiological, for example, in response to major surgery, trauma, or blood loss. Pathological activation of platelets occurs in cases of disseminated intravascular coagulation (DIC), which can be triggered, for example, by sepsis or malignancy. Activated platelets are rapidly removed from the circulation, resulting in thrombocytopenia. Patients receiving extracorporeal membrane oxygenation treatment also show increased platelet consumption.
> Greater destruction
More than 50% of cases of thrombocytopenia in critically ill patients are the result of sepsis or severe infection.
Both antiplatelet drugs and antibiotics have been reported to cause immune-mediated adverse reactions that can lead to thrombocytopenia. Together, they represent about 15% of cases in intensive care units. The formation of antibodies can also cause thrombocytopenia.
The most common example of this is the formation of antibodies against the heparin-platelet factor 4 (PF4) complex; These antibodies cause heparin-induced thrombocytopenia (HIT) when heparins are used as anticoagulants. However, this is relatively rare and is reported in <5% of patients with thrombocytopenia in intensive care units.
| Assessment, diagnosis and clinical evolution |
The underlying cause of thrombocytopenia can often be identified by taking a complete medical history and monitoring the clinical course, and performing specific laboratory diagnostic tests. In about 25% of critically ill patients with thrombocytopenia, the condition has more than one underlying cause ( Figure 1 ).
It is essential to obtain an overview of the patient’s medical history, comorbidities, and medications and then view the current clinical status in light of this information. An attempt should be made to determine whether thrombocytopenia is a result of the current critical illness and associated organ dysfunction, or whether it is part of a preexisting underlying condition, such as a serious hematologic malignancy.
The absolute platelet count should also be considered, along with the development and course of thrombocytopenia. Specific patterns will often become evident that may reveal the underlying cause ( Table 1 ). In general, thrombocytopenia will be more severe (< 50 x 10 9 /L) if a chronic underlying cause is accompanied by additional new etiologic factors; platelet transfusion may then fail to increase the platelet count. Because of high platelet turnover, low counts in critical illness likely present a lower hemostatic risk than thrombocytopenia caused by bone marrow failure.
It is also important to know other factors that may contribute to a low platelet count. Examples include pseudothrombocytopenia due to EDTA-induced platelet aggregation, hemodilution due to fluid infusion, massive transfusions of other blood components without platelets, or accumulation of platelets in the spleen in cases of splenomegaly or liver disease with portal hypertension. Patients with thrombocytopenia who develop thromboembolic disease should be tested for procoagulant conditions.
| Clinical course | probable cause |
| Platelet count low and remains low | Bone marrow failure Hypersplenism |
| Platelet count decreases rapidly, but then quickly normalizes | Surgery Use of extracorporeal circulation machine Massive transfusions without platelets |
| Gradual decrease and normalization of platelet count as clinical status improves | Septicemia Pancreatitis Inflammatory conditions |
| The platelet count drops and remains low despite the patient’s clinical improvement | Drug-induced thrombocytopenia |
| Platelet count falls and remains low in patients with persistent organ failure | Septicemia Disseminated intravascular coagulation (DIC) Circulatory insufficiency |
Table 1. Typical clinical courses of thrombocytopenia in critically ill patients and possible underlying causes.
| Treatment |
In critically ill patients, thrombocytopenia or a rapid drop in platelet count are markers of poor prognosis and increased risk of mortality.
The patient’s underlying condition must be treated. Infection control and organ supportive therapy should be prioritized if thrombocytopenia is caused by sepsis, while hemostasis and blood transfusions are appropriate if thrombocytopenia is the result of massive hemorrhage.
Providing the correct treatment depends on identifying the causes. Platelet transfusion may be the correct approach in patients with conditions that reduce production or increase consumption/destruction of platelets, but may be potentially harmful in conditions where there is increased intravascular activation, such as heparin-induced thrombocytopenia, thrombotic thrombocytopenic purpura, or prothrombotic disseminated intravascular coagulation.
Platelet transfusion may also increase the risk of nosocomial infections and transfusion-related (acute) lung injuries.
These factors justify a conservative approach to the use of platelet transfusions, with more emphasis on treating the underlying condition.
> Therapeutic transfusion
To avoid severe thrombocytopenia and hemodilution of coagulation factors, severe bleeding should be treated with a balanced transfusion of red blood cells, plasma, and platelets. According to international guidelines, platelet transfusion should be considered for critically ill patients with bleeding and a platelet count < 50 x 10 9 /L, or in whom reduced platelet function is suspected/confirmed.
> Prophylactic transfusion
The most common reason for giving platelet transfusions to critically ill patients is to prevent bleeding.
Clinical practice varies considerably, but international guidelines recommend platelet transfusion if the count is < 10 x 10 9 /L. It is estimated that transfusion increases the platelet count by about 15 x 10 9 /L per unit of transfusion, although this can vary to a relatively large extent.
> Transfusion related to procedures
Platelet transfusion is recommended to minimize the risk of bleeding during certain procedures, for example, during implantation of a central venous catheter in patients with a platelet count of < 20 x 10 9 /L. Likewise, there are guidelines and recommendations for the absolute platelet count in patients undergoing lumbar puncture or epidural anesthesia (> 50 x 10 9 /L), major surgery (> 50 x 10 9 /L) or neurosurgery (> 100 x 10 9 /L). However, these recommendations are largely based on clinical experience and the evidence base is limited.
> Other treatment methods
Drugs can affect the production and destruction of platelets. In the critically ill, steroids can be administered if a low platelet count is suspected to be of immunological origin.
Conclusions
|















