Highlights
|
Dermatoscopy has proven to be a useful non-invasive diagnostic technique for the diagnosis of cutaneous melanoma. However, the diagnostic accuracy of dermoscopy depends significantly on the degree of experience of the observers. 3 Many algorithms have been described trying to achieve a standard criterion for the evaluation of dermoscopic patterns and structures. Furthermore, the application of some algorithms could take a long time, so their efficiency and reliability in daily practice could be lower than expected.
Previous studies have shown that most melanomas differ from benign melanocytic lesions in the number of colors, asymmetry in colors or structures, and the presence of some melanoma-specific dermoscopic structures.
Based on these facts, we carried out a study to develop a dermoscopic algorithm for the diagnosis of melanoma that met the following characteristics: precision, maximum sensitivity and specificity to detect cutaneous melanoma; independence of the observer’s experience in dermoscopy; and easier to perform in daily practice than previous dermoscopic algorithms.
Aim
To propose a simplified dermoscopic algorithm for the diagnosis of melanoma.
Material and methods
A multicenter retrospective analysis of 1,120 dermoscopic images of atypical melanocytic tumors (320 melanomas and 800 non-melanomas) was performed.
An algorithm was designed based on polychromy, asymmetry in colors or structures and some specific structures of melanoma. Univariate and multivariate logistic regression analysis was calculated to estimate the coefficients of each potential predictor for melanoma diagnosis.
A score was developed based on dermoscopic evaluations performed by four experts blinded to the histological diagnosis.
Results
Most melanomas had:
- ≥3 colors (280; 84.5%)
- Asymmetry in colors or structures (289; 90.3%)
- At least one melanoma-specific structure (316; 98.7%).
PASS score ≥3 had a sensitivity of 91.9%, specificity of 87%, and diagnostic accuracy of 88.4% for melanoma. The PASS algorithm showed an area under the curve (AUC) of 0.947 (95% CI 0.935-0.959).
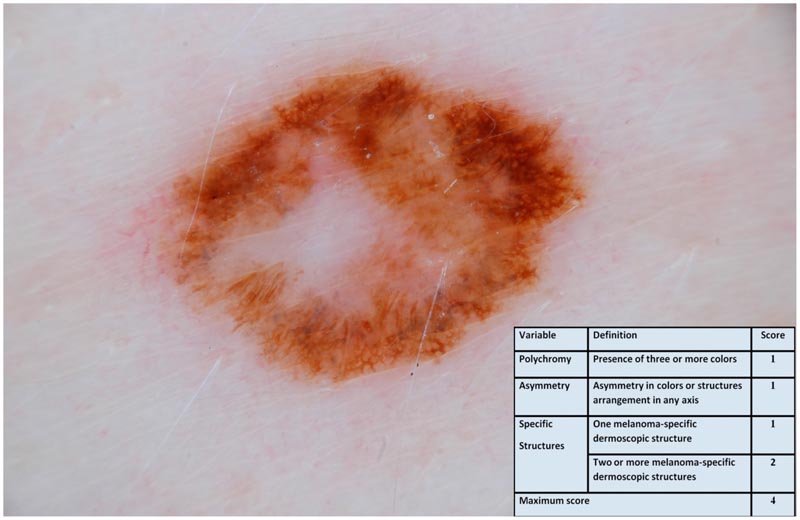
Dermoscopic image of suspicious pigmented lesions with three colors: dark brown, light brown and white (1 point); asymmetry of colors and structures (1 point); and atypical pigmented network as a melanoma-specific structure (1 point). The PASS score was 3. The histological diagnosis was superficial spreading melanoma in situ.
Limitations
This study was retrospective. A comparison between the performances of different dermoscopic algorithms is difficult due to their designs.
Conclusions
The PASS algorithm showed very good diagnostic accuracy, regardless of the experience of the observers, and appears easier to perform than previous dermoscopic algorithms.
Discussion
Dermatoscopy is a non-invasive visual diagnostic technique capable of improving the diagnostic accuracy of melanoma by up to 49% compared to visual examination. There are several algorithms for diagnosing melanoma based on the presence or absence of different colors, patterns, and dermoscopic structures in a lesion. Its objective should be to provide a series of objective and homogeneous criteria when analyzing atypical pigmented lesions and, if possible, independent of the observer’s previous experience.
The interobserver agreement analysis revealed that the identification of colors and asymmetries had a higher agreement rate than most dermoscopic structures. Previous studies have determined that features related to overall organization, colors, and symmetries have greater concordance and discrimination power than many well-known diagnostic structures, such as the atypical pigment network or irregular spots. Some dermoscopic algorithms, such as the CASH and TADA algorithms, are based on this idea. This finding has been confirmed in our concordance analysis and supports this approach.
The identification of melanoma-specific dermoscopic structures is a common basis in almost all of these algorithms but some melanomas may not present any specific dermoscopic criteria. This explains why in recent years so many structures and vascular patterns suggestive of melanoma have been described. In our study, almost all melanomas featured at least one melanoma-specific structure, and 82.5% had two or more.
In 2016, a group of researchers from the International Dermatoscopy Society (IDS) published the largest comparative study between dermoscopic algorithms to date. 7They secondarily analyzed, based on the primary analysis of certain dermoscopic structures, the diagnostic accuracy results obtained by six analytical algorithms.
The Menzies method showed the highest sensitivity for melanoma detection (95.1%, 95% CI 89.0–98.4%) and the 3-point checklist was the lowest (68.9%). , 95% CI 53.0–64.6%). The highest specificity was shown by the ABCD rule (59.4%, 95% CI 54.0-64.6%) and the lowest by the Menzies method (24.8%, 95% CI 20.1-30.1% ). No statistically significant differences were observed in the area under the ROC curve of the CASH algorithm, 7-point checklist, 3-point checklist, chaos and clues, or the ABCD rule, but the Menzies method showed a slightly lower AUC. lower (P 0.01). These results can only give us an indicative impression of the reliability of each algorithm’s criteria and should be evaluated with caution.
Other dermoscopic algorithms have also included clinical criteria such as age or tumor diameter in their diagnostic algorithms to improve their accuracy. The 18 PASS algorithm considers only dermoscopic characteristics to simplify its performance in daily practice and reduce interobserver variability, achieving very good sensitivity, specificity and precision for detecting cutaneous melanoma. Its variables form a four-letter acronym that is easy to remember and does not require complex mathematical operations as in the ABCD dermoscopic algorithm or the IDScore.
Regarding the degree of interobserver agreement , the application of the diagnostic methods was better (moderate or K ˃ 0.4) than most dermoscopic structures (acceptable or K = 0.2-0.4, with exceptions). These results are similar to those obtained in studies carried out on inexperienced observers, so they would be independent of previous training in dermoscopy. In our study we achieved moderate interobserver agreement regardless of the researchers’ experience in dermoscopy.
Trends in recent years seem to be the development of automated algorithms through the use of artificial intelligence and convolutional neural networks that increase the accuracy of melanoma diagnosis and even surpass the human observer. However, most of these studies present very heterogeneous methodologies, and a prospective controlled study has shown that the degree of diagnostic accuracy decreases drastically when applied in real-life conditions.
Final message We propose a simplified dermoscopic algorithm for the diagnosis of melanoma. The PASS algorithm is based on polychromy, asymmetry of colors and structures, and some specific structures of melanoma. This algorithm achieves very good diagnostic accuracy, regardless of the experience of the observer, and seems easier to perform in daily practice than other previous dermoscopic algorithms. |
















