| SUMMARY |
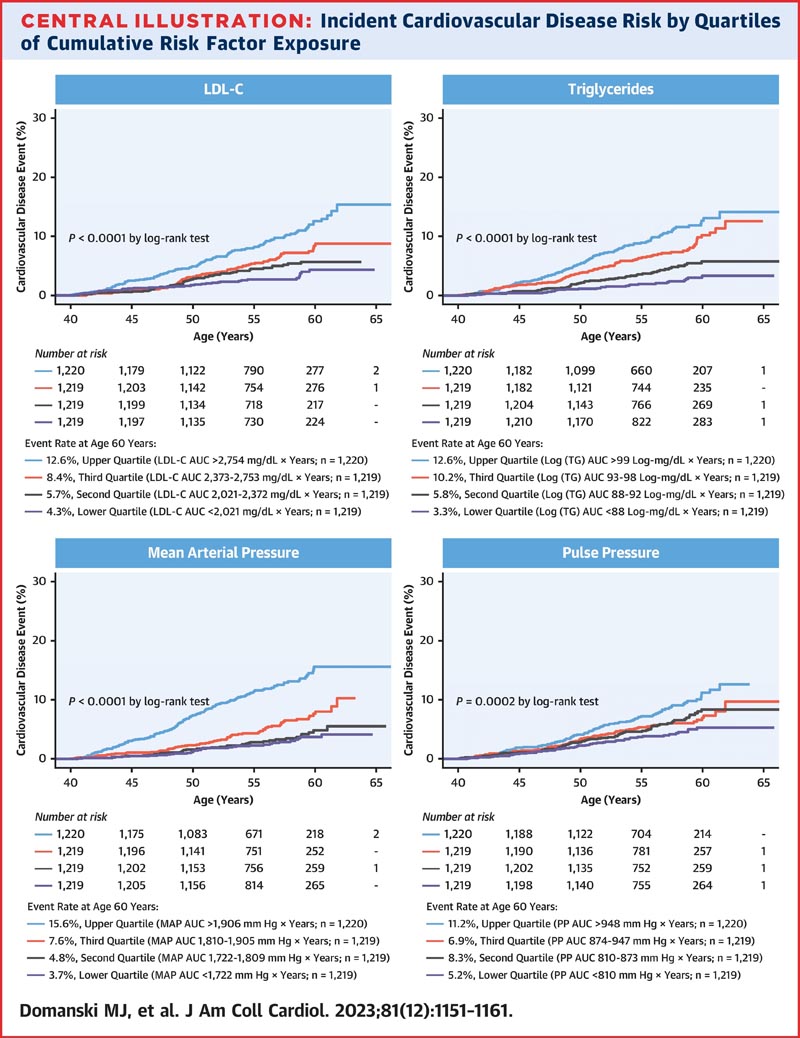
> Background The quantitative relationship of incident cardiovascular disease (CVD) with cumulative lifetime exposure to risk factors is not well understood. > Objectives Using data from the CARDIA (Coronary Artery Risk Development in Young Adults) study, we examined the quantitative associations of cumulative exposure over time to multiple risk factors operating simultaneously with the incidence of CVD and the incidence of its components. > Methods Regression models were developed to quantify the influence of the time course and severity of multiple CVD risk factors, operating simultaneously, on the risk of incident CVD. Outcomes were incident CVD and the incidence of its components: coronary heart disease, stroke, and congestive heart failure. > Results Our study included 4958 asymptomatic adults enrolled in CARDIA between 1985 and 1986 (ages 18 to 30 years) who were followed for 30 years. The risk of incident CVD depends on the time course and severity of a number of independent risk factors, the impact of which is mediated by their effects on individual components of CVD after age 40 years. Cumulative exposure ( AUC vs. time) to low-density lipoprotein cholesterol and triglycerides was independently associated with the risk of CVD incidence. Of the blood pressure variables , the areas under the mean arterial pressure versus time curve and the pulse pressure versus time curve were strongly and independently associated with the risk of incident CVD. |
| Conclusions |
Quantitative description of the link between risk factors and CVD informs the construction of individualized CVD mitigation strategies, the design of primary prevention trials, and the evaluation of the public health impact of risk factor-based interventions.
| Comments |
UM School of Medicine faculty develop tool to assess risk earlier in vulnerable patients.
Since heart disease is the most common cause of death worldwide, researchers have sought to quantify how cumulative exposure to multiple risk factors, such as high blood pressure, obesity, and high cholesterol, affect an individual’s risk of heart disease. a heart attack or stroke. Using sophisticated modeling techniques, researchers at the University of Maryland School of Medicine (UMSOM) have developed a new tool that can predict the risk of heart disease in people over the age of 40 based on their total exposure, over time. of the years, to risk factors for heart disease.
The new research findings, published in March in the Journal of the American College of Cardiology , used data from Coronary Artery Risk Development in Young Adults (CARDIA), which recruited about 5,000 healthy young adults from four U.S. cities. and followed them for 30 years. . The researchers were able to calculate from these data the cumulative effect of individual risk factors, such as high blood pressure, diabetes, high cholesterol, and the additive effects of multiple risk factors that can cause cardiovascular disease.
Black patients were found to have a 46 percent higher risk of developing heart disease compared to white patients. This finding is independent of other risk factors, including family history, smoking habits, and college attendance (a marker of socioeconomic status). Black patients were also found to be more susceptible to the cardiovascular effects of uncontrolled high blood pressure compared to white patients. White patients, on the other hand, were found to be more susceptible to elevated levels of low-density lipoprotein (LDL) than black patients.
"These data make clear the importance of instituting risk factor reduction strategies as early as possible in life to reduce cumulative time-related exposure to harmful risks," said the study’s lead author, Michael J. Domanski. , MD, professor of medicine at UMSOM. . "These results suggest that a self-reported black racial status is a marker of underlying and unexplained differences in risk factor impact."
The results of this study could help guide clinicians in developing personalized prevention strategies for individual patients. Public health policymakers could also use the new risk calculation tool to assess the likely impact of proposed heart disease prevention programs, while researchers could use it to help design clinical trials to test heart disease prevention strategies. heart diseases.
"By examining the long-term impact of multiple risk factors on cardiovascular disease, our study highlights the importance of cumulative exposure in determining an individual’s risk," said Xin Tian, PhD, associate professor at UMSOM and biostatistician at the National Heart, Lung, and Blood Institute (NHLBI), part of the National Institutes of Health (NIH). "Our findings underscore the need for personalized prevention strategies that address both the time course and severity of these risk factors. As scientists, it is our duty to use this knowledge to inform the development of effective prevention and intervention strategies that can reduce the burden of cardiovascular disease on individuals and society as a whole.
The R Shiny app, developed in this study, is a tool that allows medical providers to insert cardiovascular risks, patient history, and patient race to determine individual risks and how best to address them. Electronic medical records are now widely available, making the development of tools like the R Shiny app possible. R Shiny can be used to estimate cardiovascular risks after age 40 based on the severity of risk factors in adulthood. The application is hosted on the NHLBI website.
“Our study demonstrates the power of innovative statistical data science approaches to enable biomedical researchers to gain deeper insights into complex health problems, such as cardiovascular disease. We were able to develop risk prediction models that provide a more accurate and personalized assessment of an individual’s risk,” said Colin Wu, PhD, associate professor of medicine at UMSOM and mathematical statistician at the NHLBI, part of the NIH.
During the two-decade follow-up period after age 40, researchers found that 316 people in the study experienced their first cardiovascular event, including heart disease, stroke, and congestive heart failure.
“Cardiologists could use this new tool to convince patients to take steps to reduce their risk of heart attack or stroke by quantifying how much their risk would improve if they better controlled, for example, their cholesterol and hypertension,” Mark said. . Gladwin, MD, Dean of the University of Maryland School of Medicine, Vice President for Medical Affairs at the University of Maryland, Baltimore, and John Z. and Akiko K. Bowers Distinguished Professor. “That could have a significant impact, particularly on vulnerable populations who have not been aggressively treated for cardiovascular risks in the past due to long-standing health inequalities.”
The Cardia data used for this research is supported by NHLBI in collaboration with the University of Alabama at Birmingham (HHSN268201800005I and HHSN268201800007I), Northwestern University (HHSN268201800003i), House of HHSN2682018006I). 68201800004i).
















