Debunking a myth. You know the "Korotkoff sounds" of blood pressure, first described in 1905 to measure blood pressure. It was thought that they came from the brachial artery, but this is not the case: they come from vibrations of the surrounding tissue.
Summary
Blood pressure measurement is the most widely used clinical test to predict mortality risk. The gold standard for its non-invasive evaluation is the auscultatory method, which is based on listening to the so-called "Korotkoff sounds" in a stethoscope placed at the outlet of a pneumatic cuff. However, more than a century after their discovery, the origin of these sounds is still the subject of debate, which implies a series of clinical limitations.
We image Korotkoff sound (KS) generation in vivo at thousands of images per second using ultrafast ultrasound. We demonstrate both with experience and theory that Korotkoff sounds (KS), paradoxically , are not sound waves emerging from the brachial artery, but rather shear vibrations transmitted to the surrounding tissues through nonlinear propagation of the pulse wave. . When these shear vibrations reached the stethoscope, they were synchronous, correlated, and comparable in intensity to Korotkoff (SK) sounds.
Understanding this mechanism could ultimately improve blood pressure measurement and provide additional insight into arterial mechanical properties.
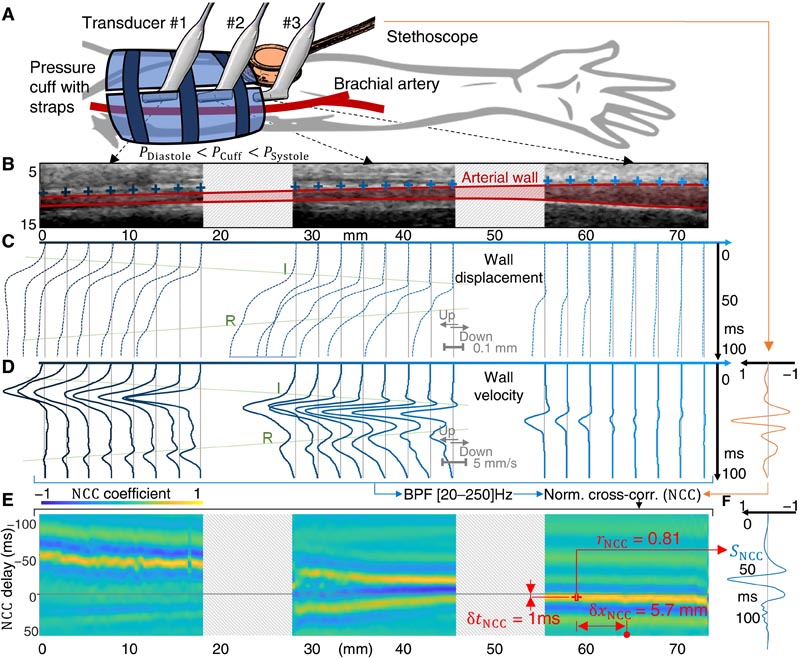
Fig. 1. The temporal evolution of arterial wall velocity under the stethoscope is highly correlated with SK . (A) Experimental setup. (B) B-mode images corresponding to the positions of the three transducers, with dashed pads corresponding to the unimaged sections between each position. The lumen of the brachial artery is identified in red. Blue crosses identify 24 points on the upper wall. (C) Corresponding axial displacement and (D) axial velocity time courses. I, incident pulse wave; R, reflected wave. The KS of the stethoscope is plotted in orange. (E) NCC of the band-pass filtered velocity time courses and the KS. rNCC is the maximum of the NCC, corresponding to a distance δxNCC to the center of the probe and a signal delay of δtNCC. The time course of the corresponding SNCC wall velocity is reported in blue in (F).
Discussion
From these results, we propose the following theory for the origin of Korotkoff (SK) sounds:
(i) By decreasing the transmural pressure and therefore the stiffness of the brachial artery, the pressure cuff slows down the pulse wave and amplifies local displacements of the arterial wall.
(ii) The resulting high arterial wall velocity compared to the pulse wave propagation velocity results in a highly nonlinear propagation regime under the cuff that transfers wave energy from very low, barely audible frequencies. , at a higher frequency audible content.
(iii) These nonlinear vibrations radiate to the surrounding tissues , where they form shear displacements with an amplitude that decays exponentially with distance from the arterial wall. These tissue vibrations propagate together with the arterial pulse wave.
Perspectives for pressure measurements.
Answering the question about the origins of KS could have important clinical consequences. Even if the auscultation method tends to be replaced by automatic oscillometric assessment, the latter has well-known limitations that can lead to underestimation or overestimation of BP. KS remain the calibration reference for these commercial devices with undisclosed algorithms, so understanding their mechanism is essential for BP measurements. In particular, accurately estimating DBP is challenging.
Essentially, our findings show that the disappearance of SK with decreasing cuff pressure is a gradual phenomenon. Not only does the intensity of the KS decrease when the cuff pressure reaches the diastolic blood pressure (DBP), but we also demonstrate that the frequency content of the KS is driven by the nonlinear propagation of the pulse wave.
Therefore, around the DBP, where the nonlinear behavior is less pronounced, the arterial wall velocity has a very low pitch spectral content, in a range where the human ear has very low sensitivity. This dependence of frequency content on propagation distance also explains why the position of the stethoscope can also influence the perception of KS. In general, KS become weaker and deeper around the DBP value, which may explain why it is frequently overestimated , especially in hypertensive participants.
















