Multi-organ evaluation in mainly non-hospitalized people after SARS-CoV-2 infection: the Hamburg City Health Study COVID program
As of December 2021, the coronavirus disease 2019 (COVID-19) pandemic has resulted in more than 260 million confirmed positive cases of severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) worldwide.
In Europe, 3.6% of infected patients required intensive care, 90% recovered in an outpatient setting.
Severe COVID-19 can affect multiple organ systems during the acute phase of the disease. Deterioration of lung, heart, and kidney function, as well as thromboembolism, have been described in severely ill and deceased patients. Additionally, serious neurological complications have been reported, including cerebrovascular events, encephalopathy, and encephalitis.
While individual reports describe persistent symptoms of pulmonary, renal, cardiac or vascular dysfunction, as well as fatigue or depression arising mainly from hospitalized cohorts, a systematic investigation, especially of subclinical changes of the structure and function of multiple organs, is of particular interest. in the current study. pandemic context.
With this study, we aimed to comprehensively determine the medium-term impact of a mild to moderate course of COVID-19 on specific organ function. A COVID-19 disease course was classified as mild to moderate when it did not require treatment in the intensive care unit.
We assessed multi-organ function by deep phenotyping in patients ∼9 months after recovery from COVID-19 in direct comparison with age-, sex-, and education-matched subjects from a population-based cohort study.
Goals
Long-term sequelae may occur after SARS-CoV-2 infection. We comprehensively evaluated organ-specific functions in individuals after mild to moderate SARS-CoV-2 infection compared to general population controls.
Methods and results
Four hundred and forty-three people, mainly non-hospitalized, were examined at a median of 9.6 months after the first positive SARS-CoV-2 test and matched for age, sex and education with 1,328 controls from a German cohort based on the population. We evaluate pulmonary, cardiac, vascular, renal, and neurological status, as well as patient-related outcomes.
Body plethysmography documented slightly lower total lung volume (regression coefficient -3.24, adjusted P = 0.014) and higher specific airway resistance (regression coefficient 8.11, adjusted P = 0.001) after SARS-CoV-2 infection.
Cardiac evaluation revealed slightly lower measures of left (regression coefficient for left ventricular ejection fraction on transthoracic echocardiography −0.93, adjusted P = 0.015) and right ventricular function and higher concentrations of cardiac biomarkers (factor 1.14 for high-sensitivity troponin, 1.41 for N-terminal B-type natriuretic peptide, adjusted P ≤ 0.01) in post-SARS-CoV-2 patients compared with matched controls, but no significant differences in the findings of cardiac magnetic resonance imaging.
Sonographically non-compressible femoral veins , suggesting deep vein thrombosis, were substantially more common after SARS-CoV-2 infection (odds ratio 2.68, adjusted P < 0.001).
Glomerular filtration rate (regression coefficient −2.35, adjusted P = 0.019) was lower in post-SARS-CoV-2 cases.
Relative brain volume , prevalence of cerebral microbleeds, and infarct residuals were similar, while mean cortical thickness was greater in post-SARS-CoV-2 cases.
Cognitive function was not affected. Similarly, patient-related outcomes did not differ.
Conclusion
Subjects who appear to have recovered from mild to moderate SARS-CoV-2 infection show signs of subclinical multiorgan involvement related to pulmonary, cardiac, thrombotic, and renal function without signs of structural brain damage, neurocognitive impairment, or quality of life. The respective evaluation can guide the subsequent management of the patient.
Discussion
In more than 1,700 individuals, we extensively evaluated the specific structure and function of multiple organs and explored neurocognitive and PRO to comprehensively evaluate the long-term intermediate effects of mild and moderate COVID-19 disease. We consistently see subclinical organ-specific involvement ( Graphical Summary ).
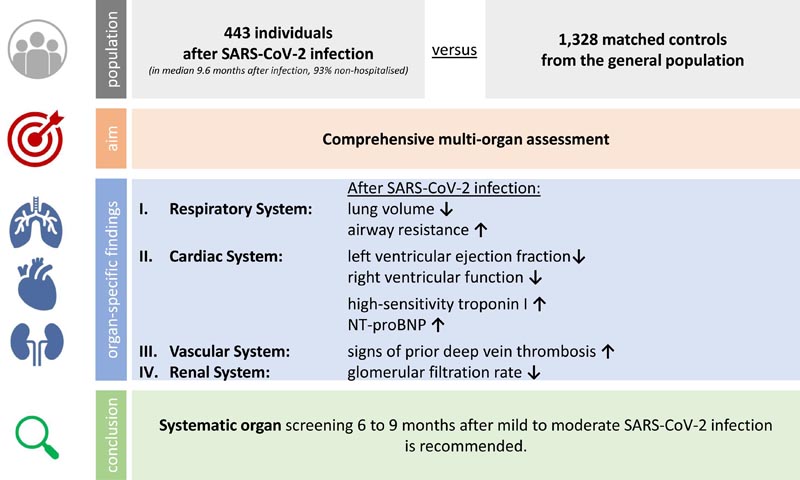
The key question is: How does a mild to moderate course of SARS-CoV-2 infection in mainly non-hospitalized people affect specific organ functions in the medium term compared to the general population? The key findings are (i) a mild to moderate course of SARS-CoV-2 infection is associated with subsequent signs of subclinical multiorgan involvement; (ii) the associations mainly affect the pulmonary, cardiac, coagulation and renal systems; and (iii) no systematic associations were observed with structural brain damage, neurocognition, or quality of life. The take-home message is that routine screening for multi-organ function is recommended even after mild to moderate SARS-CoV-2 infection to identify those at risk and initiate appropriate preventive therapies.
Autopsy studies indicate that SARS-CoV-2 affects multiple organs beyond the respiratory tract, including the heart, brain, and kidneys. Some patients continue to suffer from heterogeneous symptoms after the acute phase of critical illness. These conditions are described as ’post-COVID-19 syndrome’ or, if symptoms continue for more than 6 months, as ’long COVID-19 syndrome’.
Clinical, imaging, or laboratory findings should accompany the diagnosis of subsequent or long-term COVID-19. To date, the long-term effects following a mild to moderate course of COVID-19 disease remain largely unknown. It is important to perform a systematic and comprehensive examination of possible multiorgan impairment to plan surveillance and possible diagnostic tests after recovery.
While there is evidence that post-COVID-19 patients with mild to moderate disease have preserved lung volumes, we found significantly lower total lung volume (TLC) in subjects after mild to moderate infection compared to controls. This is in line with previous findings of a reduction in TLC starting after mild COVID-19.
Residual inflammatory processes or the onset of subclinical fibrotic remodeling could explain the slightly lower lung volumes observed in the post-SARS-CoV-2 cohort. Consistent with histological findings, we found increased airway-specific resistance in participants after SARS-CoV-2 infection. Evaluation of lung function after recovery from COVID-19 should be considered at the slightest suspicion, even in apparently healthy individuals (Figure 2).
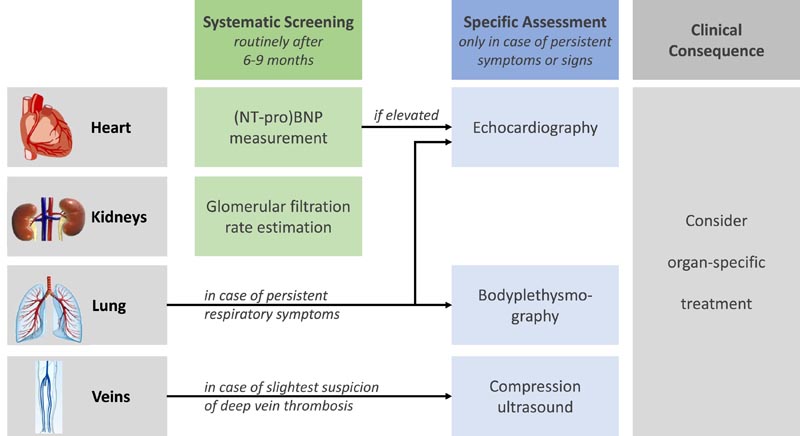
Suggested standardized clinical examination after a mild to moderate course of SARS-CoV-2 infection. (NT-pro)BNP, (N-terminal pro-)B type natriuretic peptide.
From a cardiovascular perspective , a numerically small reduction in left ventricular ejection fraction with a difference of 1% to 2% was observed in participants after SARS-CoV-2 infection, accompanied by an increased concentration of cardiac biomarkers. reflecting modest myocardial involvement.
In a very long-term perspective, even a small reduction in left ventricular function and a slight increase in NT-proBNP concentration translates into an increased risk of mortality in the general population. Therefore, determination of NT-proBNP , followed by echocardiographic monitoring in case of elevated concentrations, may be recommended after recovery from COVID-19 to avoid untreated cardiac dysfunction.
More importantly, our data suggest a significantly higher prevalence of deep vein thrombosis in participants after SARS-CoV-2 infection. Although affected by some examiner bias, compression ultrasound is commonly accepted and widely used as a reference standard in daily clinical practice. The present findings expand the rapidly growing evidence of an association between COVID-19 and venous thromboembolism, while adding a prospectively recruited cohort with mild or moderate disease.
Of note, levels of coagulation parameters assessed at a median of 9.6 months after mild to moderate SARS-CoV-2 infection did not differ compared to matched controls. Therefore, we can assume that the acute thrombotic events themselves, associated with the activation of the coagulation and fibrinolytic cascade, occurred much earlier during the course of COVID-19.
In this context, the non-compressible veins observed in our study should be interpreted as remnants of the fibrotic processes that replace the previous thrombotic material. Considering the existing evidence, the results of the current study suggest that guideline-based surveillance with active detection of deep vein thrombosis should be considered in case of early minimal clinical suspicion during COVID-19 infection.
Arterial system assessment indicated more frequent carotid plaques in post-SARS-CoV-2 participants compared to matched controls, while CIMT was comparable between groups.
People after recovery from SARS-CoV-2 were also found to have a subtle decline in kidney function compared to matched controls, which also does not appear clinically relevant at the time of the investigation. However, autopsy studies have shown distinct renal tropism related to SARS-CoV-2 and early urinary abnormalities associated with mortality and multi-organ failure in hospitalized patients with COVID-19.
Therefore, the differences observed in our study could reflect a specific SARS-CoV-2-related lesion with an onset trajectory towards early chronic kidney disease, being an important risk factor for mortality and cardiovascular events. Therefore, we advocate a follow-up evaluation of a renal function marker for 6 to 9 months, even after mild SARS-CoV-2 infections.
Brain MRI was available in a large subgroup of patients and did not reveal any signs of increasing vascular brain damage. The presence and number of brain microbleeds and white matter hyperintensities as the most common hallmark of small blood vessel disease were comparable between participants recovered from mild to moderate COVID-19 and controls.
Central parameters such as depression, anxiety and quality of life were tested . In none of the five scales were significant differences observed in the main analysis. However, in an exploratory subgroup analysis, higher degrees of depression and anxiety were observed in subjects with a moderate course of COVID-19 compared to subjects with no or mild symptoms.
These findings extend and corroborate previous work describing prolonged severe COVID-19 symptoms after intensive care courses of COVID-19, which also affect the psychosocial domain. People after a mild to moderate illness may have normalized their previously elevated levels of anxiety and depression at the time of the survey.
In conclusion , in the HCHS COVID project, we demonstrated that patients who apparently recovered from mild to moderate COVID-19 suffer from a modest subclinical multi-organ condition related to thrombotic, pulmonary, cardiac and renal function without signs of structural brain damage, obvious impairment of cognitive function or quality of life. While the impact on very long-term outcome remains unclear, standardized clinical examination of these conditions after recovery is recommended. |
















