Highlights • Intensive lifestyle therapy (ILT) in the workplace causes marked weight loss. • ILT markedly improves β-cell function and insulin sensitivity of multiple organs. • Metabolic effects are associated with changes in the biology of muscle and adipose tissue. |
The increase in the prevalence of obesity in recent decades has led to a marked increase in the prevalence of type 2 diabetes (T2D). Consequently, T2D has become a major global public health problem due to its causal relationship with serious medical complications, adverse effects on physical function, and considerable economic impact related to increased healthcare costs and decreased of productivity.
Lifestyle therapy consisting of decreasing dietary energy intake and increasing physical activity with concomitant weight loss is the cornerstone of treatment for patients with obesity and T2DM. Weight loss has a dose-dependent therapeutic effect on metabolic function and glycemic control in people with prediabetes and T2D. Additionally, diabetes remission (HbA1c < 6.5%) without diabetes medications often occurs after 15% to 20% weight loss in those without long-standing T2D or severe cell dysfunction. β.
Regular exercise, particularly the combination of resistance exercise, is an important component of lifestyle therapy in people with T2D because it has therapeutic effects on glycemic control that are independent of weight loss.
Providing effective lifestyle intervention is often challenging due to the limited availability of evidence-based programs, high cost, and inconvenience to participants.
The workplace environment offers a unique opportunity for lifestyle therapy because it can reduce or eliminate many of these barriers and further improve compliance by providing social support associated with a group setting.
Although a systematic review of workplace-based weight loss programs and subsequent individual studies found that workplace interventions resulted in modest weight loss and no program achieved the large weight loss needed to induce remission of diabetes, most interventions in these studies were low or moderate intensity and provided minimal supervision (contact less than once a month), and only one program included supervised exercise sessions. We are not aware of any studies evaluating the potential therapeutic effect of an intensive diet and supervised exercise intervention conducted in a workplace setting.
The purpose of the present study was to conduct an 8-month randomized controlled trial in people with obesity and T2D to determine the therapeutic effects of intensive lifestyle therapy (ILT) that involved both dietary energy restriction such as supervised physical training conducted in the workplace compared to standard care (dietary and physical activity instructions as recommended by American Diabetes Association [ADA] guidelines); American Diabetes Association, 2020).
The effects on (1) the main factors involved in the pathogenesis of T2D (insulin sensitivity, β-cell function and the metabolic response to glucose intake), (2) body composition, (3) function were analyzed. (cardiorespiratory fitness and muscle strength), (4) plasma concentrations of adipokines that could influence insulin action (adiponectin and plasminogen activator inhibitor-1 [PAI-1]), and (5) potential cellular mechanisms that supposedly affect insulin action (gene expression profile of skeletal muscle and mitochondrial function, and expression in adipose tissue of genes involved in extracellular matrix [ECM] formation and inflammation).
We hypothesized that the improvement in whole-body insulin sensitivity (primary outcome) and all major factors involved in the pathogenesis of T2D (secondary outcomes) would be much greater in the ILT group than in the standard care (SC) group. ).
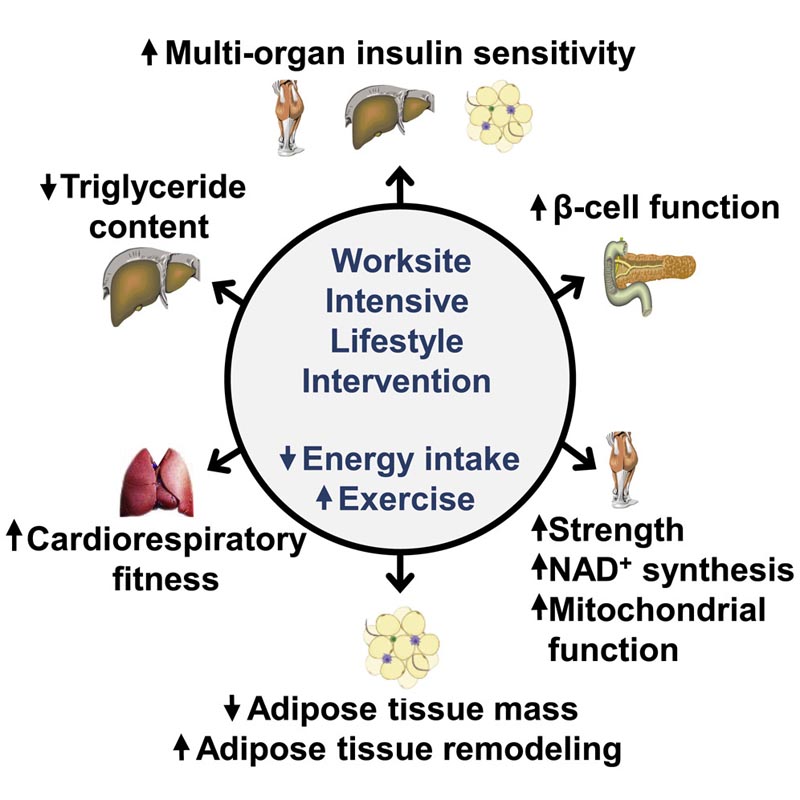
Graphic summary
Summary
Lifestyle therapy (energy restriction and exercise) is the cornerstone of therapy for people with type 2 diabetes (T2D), but it is difficult to implement. We conducted an 8-month randomized controlled trial in people with obesity and T2D (17 women and 1 man) to determine the therapeutic effects and potential mechanisms of intensive lifestyle therapy on cardiometabolic function.
Intensive workplace lifestyle therapy was conducted to improve compliance and resulted in:
- Marked weight loss (17%)
- Beneficial changes in body fat mass
- The content of intrahepatic triglycerides.
- cardiorespiratory fitness
- Muscle strength.
- Glycemic control.
- The function of β cells.
- Multiorgan control of insulin sensitivity, which were associated with changes in muscle NAD, sirtuin signaling, mitochondrial function, and adipose tissue remodeling.
These findings demonstrate that intensive lifestyle therapy delivered in the workplace has profound clinical and physiological therapeutic effects in people with T2D, which are likely mediated by specific alterations in skeletal muscle and adipose tissue biology.
Discussion
Diet-induced weight loss and increased physical activity are considered the cornerstone of therapy for people with obesity and type 2 diabetes (American Diabetes Association, 2020). However, providing an effective lifestyle intervention is often difficult due to lack of provider experience or programs, patient inconvenience, cost, and lack of compliance. The results of the present study demonstrate that ILT administered in the workplace (1) causes marked weight loss and beneficial changes in body composition (decrease in body fat mass, intra-abdominal adipose tissue volume, and intrahepatic triglyceride content without a decrease in FFM or appendicular). lean mass); (2) increases cardiorespiratory capacity and muscle strength; (3) improves glycemic control (decrease in postprandial and fasting plasma glucose, HbA1c, and use of diabetes medications) and may induce diabetes remission; (4) improves the main physiological factors involved in the pathogenesis of type 2 diabetes, namely, β-cell function and multi-organ insulin sensitivity; (5) causes beneficial cellular changes in skeletal muscle and adipose tissue biology; and (6) reduces circulating PAI-1, which is likely a mediator of systemic insulin resistance.
We conclude that marked weight loss and increased physical activity can be achieved through workplace ILT, which has profound clinical, physiological, and cellular therapeutic effects in people with obesity and T2D. Therefore, an intensive low-calorie diet and exercise intervention should be considered a primary therapy from “day 1” to treat and reverse T2D. Furthermore, our data demonstrate that an effective intensive lifestyle program can be implemented in the workplace , which has important implications for national dissemination in the management of people with obesity and T2D.
Multiorgan insulin resistance is the most common metabolic complication of obesity and is involved in the pathogenesis of dyslipidemia, nonalcoholic fatty liver disease, and T2D.
Weight loss in people with obesity improves insulin sensitivity of multiple organs ; Even moderate weight loss (i.e., 5%) improves insulin action in the liver, adipose tissue, and skeletal muscle, and progressive amounts of weight loss cause corresponding progressive increases in insulin sensitivity in multiple organs. Weight loss generally improves hepatic insulin sensitivity before skeletal muscle insulin sensitivity in people with T2D, contributing to early improvements in glycemic control.
Regular exercise , independent of weight loss, also has beneficial effects on hepatic, adipose tissue, and skeletal muscle insulin sensitivity, and the combination of resistance and aerobic exercise has greater therapeutic effects than either alone in glycemic control in people with T2D.
In the present study, we attempted to maximize the effects of lifestyle therapy on multiorgan insulin sensitivity by combining marked diet-induced weight loss with resistance training and aerobic exercise, which increased sensitivity to insulin from the liver, adipose tissue and the whole body. 100%–150%. Our data suggest that alterations in skeletal muscle and adipose tissue biology and a decrease in circulating PAI-1 are likely involved in mediating the marked improvement in insulin action.
















