| Background |
Congenital idiopathic clubfoot or clubfoot, also known as congenital talipes equinovarus, is the most common serious musculoskeletal birth defect occurring in the United States and the world .
Idiopathic clubfoot occurs in otherwise normal infants and must be distinguished from syndromic and neurogenic clubfoot, which occurs in infants as part of a neurological syndrome or condition.
Syndromic and neurogenic clubfoot are less common, are more difficult to treat, and have higher recurrence rates during and after treatment. Although syndromic and neurogenic clubfoot are important to the pediatrician, the focus of this report is on common idiopathic clubfoot.
The incidence of idiopathic clubfoot is approximately 1 to 2 per 1,000 births, resulting in 150,000 to 200,000 children with clubfoot worldwide each year. Approximately 80% of children with clubfoot are born in resource-limited countries,1–5 and approximately 2100 children born in the United States have clubfoot annually.
There are different rates of occurrence among different ethnicities. Rates have been reported as high as 7 in 1000 in Hawaiian and Maori children, 2 in 1000 in children in Malawi, 1 to 2 in 1000 in white children, and 0.5 to 1 in 1000 in Japanese and Filipino children. There is a 2:1 preponderance in males, and 30% to 50% are bilateral.6
Idiopathic clubfoot is typically an isolated congenital abnormality and is secondary to multifactorial environmental genetics and strong genetic factors.1–3,7–11 In support of a genetic cause, there is a 35% concordance in affected identical twins.12
If a parent has a clubfoot or a child in a family is born with a clubfoot, the chance of a second child in that family with a clubfoot increases to 1/35.2 Why are men affected by clubfoot twice as often? than women is unclear.2,10 A polygenic threshold model has been proposed in which the environment and multiple genes interact to produce the deformity.10
Botfoot is not a deformity secondary to third trimester intrauterine crowding and should not be confused with the much more common benign positional foot and leg deformities that often resolve without treatment, including metatarsus adductus, calcaneus valgus, and positional cavovarus.2
Early amniocentesis before 13 weeks of gestation and oligohydramnios in critical gestational periods are environmental factors that were found to be associated with idiopathic clubfoot.13,14
| Prenatal diagnosis |
Botfoot deformity can be discovered during prenatal ultrasound.
Clubfoot can be detected at 13 weeks of gestation using transvaginal ultrasound15,16 and at 16 weeks of gestation using transabdominal ultrasound.17 Visualization of a clubfoot on prenatal ultrasound requires a complete examination to evaluate additional findings indicating a clubfoot. syndromic or neurogenic bot.
Syndromic or neurogenic clubfoot patients and, less commonly, isolated clubfoot have higher rates of genetic abnormalities, which can be evaluated with fetal genetic testing.18 For example, the fetal akinesia deformation sequence has associated abnormalities that They can be detected on ultrasound, leading to more complete genetic testing.19 If syndromic clubfoot is diagnosed, referral for fetal MRI is suggested to reliably evaluate associated findings.20
Most often, prenatal diagnosis of clubfoot will occur at the routine ultrasound appointment at 20 weeks’ gestation, unless the pregnancy is being followed closely for other reasons. At this time, parents can ask the pediatrician for information or treatment advice. Prenatal treatment is not available for clubfoot; however, appropriate prenatal counseling is important. It is very helpful for parents if their pediatrician or obstetrician recommends a doctor who has experience with the Ponseti technique.
Parents can be comforted with accurate information and reliable resources that are available on the Internet, but they may also encounter confusing and inaccurate information. Pediatric orthopedic surgeons are frequently willing to meet with parents in the prenatal period to review imaging studies, assess severity, and describe treatment options.
It is best for patients to be seen by a doctor with training and experience in the Ponseti method. In areas without pediatric orthopedic surgeons and non-orthopedic surgeons experienced in clubfoot treatment, it is suggested that patients travel for care.
A prenatal diagnosis cannot always be made, even with a high-quality ultrasound, particularly if the deformity is mild or moderate. In contrast, a mild isolated clubfoot seen on prenatal examination may not be a true clubfoot at birth; It may be a positionally resolving deformity, and the false-positive rate of idiopathic clubfoot on prenatal ultrasound is estimated at 19%.21,22 It is important to note that the severity of clubfoot can be determined by ultrasound. The severity can only be determined by clinical examination of the foot.
| Newborn screening |
Evaluation of a newborn with clubfoot deformity involves a thorough general examination to determine general health and development, exclude neurologic syndromes and conditions (e.g., spina bifida, arthrogryposis, limb formation abnormalities), and provide a focused examination of the foot and limb. Examination of all joints for range of motion and stability, including the hips, is important, as is examination of the lower extremities for equal length and symmetry.
The severity of a newborn’s foot deformity is determined more by the flexibility of the foot than by its appearance.23,24
Newborn foot deformities that can be easily manipulated with an overcorrected position are considered positional rather than true botfoot. These resolve with minimal or no treatment. Unless a limb deficiency such as fibular hemimelia, tibial hemimelia, or congenital short femur is noted, radiography is not necessary.25
Several syndromes are known to be associated with clubfoot, including classic arthrogryposis, multiple pterygium syndrome, distal arthrogryposis, amniotic band syndrome, and Freeman-Sheldon syndrome.26–28
Geneticists can help evaluate patients when a syndrome is suspected. Neurological causes include myelomeningocele, lipomeningocele, tethered cord syndrome, diastematomyelia, and sacral agenesis. Careful examination of the spine is necessary to detect subtle findings associated with tethered cord, such as a sacral dimple or a patch of hair.
An infant with an isolated idiopathic clubfoot has a completely normal physical examination except for the foot and leg involved. The deformity has 4 key components that can be remembered by the acronym CAVE: The midfoot has a high arch (cavus), the forefoot is bent inward (adductus), the heel is turned inward (varus), and the heel points downward (equinus).
The deformity is quite rigid (not easily correctable with gentle manipulation), and the foot and calf may be slightly smaller than the opposite normal side. Untreated or recurrent clubfoot causes the child to walk on the lateral or dorsum side of the foot. Older children and adults with untreated clubfoot cannot wear standard shoes and are limited in sports and employment.
| Treatment |
Until the Ponseti technique was accepted as the superior method for treating clubfoot, many treatments became popular with good initial results for a time, only to fall out of favor when long-term results showed a high rate of recurrent deformity. stiffness and pain. The first recorded treatment of clubfoot is attributed to Hippocrates, who recommended “manipulation of the deformed foot and bandaging it in the corrected position.”29
Subsequently, other nonsurgical treatments involving casting, special shoes, orthotics, and even “wrench” correction were proposed 30,31. The immediate results were sometimes satisfactory; However, over time, the deformity almost always recurred.
During the first half of the 20th century, Hiram Kite became an enthusiastic advocate of nonsurgical treatment of clubfoot.32,33 Although his initial success was reported at 90%, the technique was lengthy, the results were not reproducible, and the deformity often recurred.34
As a result of dissatisfaction with Kite’s casting method, surgical releases for resistant clubfoot, which dramatically corrected the deformity in the short term, became popular in the last quarter of the 20th century.1,35–43 These extensive surgeries were performed from 4 to 18 months of age. These results in the short and medium term were good.40,41,43
However, with growth, healing from the surgery eventually led to decreased movement; the foot became painful, stiff and arthritic; and activities and function were limited as the child reached adolescence and adulthood.44–48
In 1948, Ignacio Ponseti at the University of Iowa developed a treatment method that used a new casting technique and minimal surgery.49 Ponseti’s methodology was clearly explained, easily understandable, and reproducible. One of the distinctions of his method was the prolonged booster phase, which decreased but did not eliminate recurrences. During the last quarter of the 20th century, while most centers had adopted extensive surgical releases for resistant clubfoot, Ponseti continued to refine his method.
The Ponseti method is based on a clear understanding of the clubfoot pathoanatomy and how it affects foot mechanics.8,9 Over the years, refinements to the Ponseti technique and improvements in stabilization have decreased the problem. of recurrence, and the method now became the standard for the treatment of botfoot.50,51
It should be noted that although this report focuses on isolated idiopathic congenital clubfoot, syndromic and neurogenic clubfoot can also be treated with the Ponseti method, although the treatment is prolonged, with higher relapse rates.52
A second non-surgical method of clubfoot treatment was developed in France and popularized and refined by Alain Dimeglio.53 The technique, known as the French functional method, also emphasizes gradual correction in childhood, with daily manipulations by a physical therapist. experienced and elastic bandages between therapy sessions. The approach also includes a prolonged period of overnight splinting and limited surgery for recurrences.
The correction time with this method is several months; The treatment is daily and much more laborious for both the family and the health professional. Although the method has some followers in Europe, unlike the Ponseti method, the long-term results of the technique are not known.
| The Ponseti treatment method |
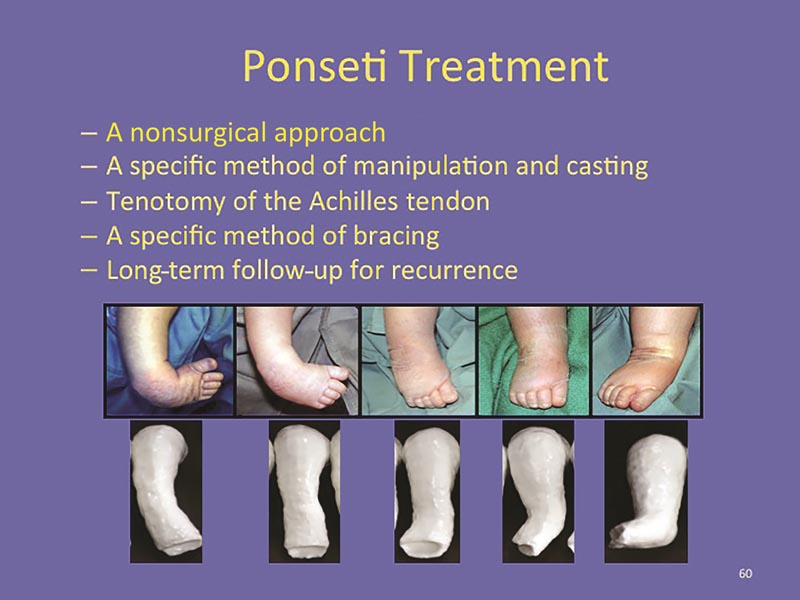
Careful and complete use of the Ponseti method leads to optimal results. The method consists of 3 treatment phases : manipulation and casting, tenotomy and stabilization.49,53–55
The first phase involves manipulation and weekly serial above-knee casting performed by a person trained in the technique. This phase usually lasts 5 to 8 casts.56,57 It is not necessary to start treatment in the newborn. Treatment can begin at any time during the neonatal period, ideally in the first 1 to 3 weeks.58
In the second phase, after all elements of the deformity except the equinus have been corrected, a percutaneous Achilles tenotomy is performed under local anesthesia by an in-clinic surgeon, which eliminates the perioperative risk of general anesthesia and concerns about the anesthetic neurotoxicity in the child.59 Some surgeons prefer to perform tenotomy in the operating room under general anesthesia, particularly in older children. A final cast is placed immediately after tenotomy and worn for 3 weeks.
Ninety percent of babies with clubfoot require a tenotomy.60 A more extensive surgical release is not necessary61. The third and most important phase is the stabilization phase, which begins immediately after removal of the post-tenotomy cast.
The corset is a foot abduction orthosis that consists of 2 shoes or splints connected by a bar. For the first 3 months, the corset is worn 23 hours per day, allowing the corset to be removed for dressing and bathing only. After the first 3 months, the brace is worn during nighttime and naptime only, with a goal of 12 to 14 hours of brace wear, until the child is 4 to 5 years old.
The principle of stabilization is that the corrected foot is maintained in an abducted and dorsiflexed position to prevent relapse. A well-designed orthotic is easily applied and removed, does not allow the foot to slip or slip, and has well-tolerated shoes (splints). In bilateral clubfoot, the shoes (splints) are externally rotated 60 to 70 degrees on the bar.
If the deformity is unilateral, the shoe (splint) on the affected side should be externally rotated 60 to 70 and the unaffected side 30 to 40. The bar should be a length between the child’s shoulders and should be fixed with the ankles in 10 to 15 degrees of dorsiflexion.
Improvements in orthotic design using shoes or splints with soft liners that can be easily detached from the bar instead of rigid shoes that are rigidly attached to the bar have made the corset much easier to wear for patients. patients and families.
Parental adherence to the booster phase of treatment has been shown to be the most important factor in preventing deformity recurrence and the ultimate success of the Ponseti method.57,62–69 It is not easy to keep a child in a brace all night, every night, for 4 years; Therefore, the ability of the pediatrician and orthopedic surgeon to motivate and support the parents to complete the stabilization program is as important as the initial correction of the deformity.
The pediatrician’s knowledge of the standard Ponseti protocol and encouragement of the family to comply and complete the booster phases of treatment are important for treatment success. Recurrence of clubfoot deformity after treatment with the Ponseti method using the traditional foot abduction orthosis ranges from 8% to 56%.67,70–73 Recurrences occur in only 6% of families who complete the procedure. stabilization, but in up to 80% of families that cannot complete the stabilization phase.74
Adherence to bracing has many factors but is not believed to be related to family upbringing, culture, or income level.75 Adherence can be improved with culturally sensitive education, a positive communication approach, and increased family awareness of braces. the importance of stabilization.76
Communication between health professionals and the family is very important for the family’s understanding of the treatment process and bracing compliance.68,77,78 Both the pediatrician and the treating pediatric orthopedic surgeon should explore barriers to adherence and empowering families to succeed.
Many treatment centers now use a clinical coordinator who instructs the family on proper use of the brace, communicates through follow-up phone calls, helps with the financial challenges of braces, and provides support in all phases of the procedure. treatment.79
| Treatment of recurrence |
Recurrence is defined as the reappearance of any of the components of the deformity.80 The first sign of recurrence is usually the development of equinus, or a tight heel cord. An inward gait develops with increased forefoot adduction, heel varus, and loss of heel strike. When the child has developed an inward or adducted gait, the recurrence is quite advanced.
If left untreated, the dynamic, flexible deformity gradually becomes more fixed. Recurrences are well treated by repeating the Ponseti method.51 Despite repeating the Ponseti method, approximately 5% to 20% of adequately treated patients with idiopathic clubfoot develop recurrences that manifest as continuous inward walking with a forefoot in adduction and flexible supination.
The deformity can be corrected with surgery limited to an anterior tibial tendon transfer.49,81–84 This is considered an early part of the Ponseti method and should not be viewed by the family as a treatment failure. Failure of the Ponseti method with residual fixed deformity requiring surgical release of the ankle or subtalar joint is rare.
| Result after treatment |
Dr. Ponseti first published his results in 1963. Of the 93 feet treated, 71% had a good result, 28% had a slight residual deformity, and only 1 had a poor result.49 These results were excellent since Unlike surgical release results, it did not deteriorate with long-term follow-up. The long-term results of the Ponseti method, as practiced at the University of Iowa, were published in 198053 and then again in 1996.54
More than 30 years after treatment with the Ponseti method, adults who had been born with a clubfoot functioned almost like a control group of adults born with normal feet. Children who underwent Ponseti treatment and had success with orthotics can be expected to participate in sports, wear normal shoes, and have excellent overall function.
The successful results of the Ponseti method have been duplicated in many other treatment centers in the United States, with reported initial correction rates of 90% to 100%.63–66,85–87
A survey by the Pediatric Orthopedic Society of America found that 97% of members use the Ponseti method as their preferred treatment for idiopathic clubfoot.5 As a result, the rate of radical surgical releases performed for idiopathic clubfoot in the United States has decreased from 70% in 1996 to 5% to 10% in 2006. Parental satisfaction at 2 years of age is more than 90% in numerous studies.88
Through computer gait analysis of children treated by the Ponseti method compared to unaffected children, researchers demonstrated good clinical outcomes with high function.89 Children treated by the Ponseti method had more ankle strength than children surgically treated; however, children who were treated for clubfoot had a small decrease in ankle power compared with normal feet.90,91 Residual inward gait was sometimes noted.
| Challenges and complications |
The Ponseti method is safe, but can have complications even when performed by experienced professionals.87 Complications include skin irritation and cast breakage. Complications of tenotomy are rare, but may include bleeding, infection, pseudoaneurysm, and damage to the neurovascular bundle.87 Minimal delays in achieving gross motor milestones are seen in children treated with the Ponseti method.92
The most common challenge to successful treatment is adherence to the entire treatment protocol. Patients and families may experience distress with bracing, difficulties related to the cost of braces, and the distance required to travel for treatment. It cannot be overstated that non-adherence to bracing will result in recurrence 100% of the time in the first year, 80% of the time in the second year, 60% of the time in the third year, and 30% of the time in the fourth year.
| Pie bot in countries with limited resources |
Although rarely seen in the United States and other industrialized countries, children born with clubfoot in resource-limited countries reach adulthood unable to wear shoes and walk on their toes with their toes pointing backward. Cultural bias and prejudice often relegate these children to a life of poverty, lack of education, and difficulty finding a marriage partner. For these individuals, botfoot correction is life-changing. Eighty percent of the nearly 200,000 children born with clubfoot worldwide each year are from resource-limited countries.4
The Ponseti method is particularly suitable for use in resource-limited countries because monitoring of casting and bracing can be performed by other healthcare workers rather than doctors. The results of treatment by physiotherapists trained in the Ponseti method are as good, if not better, than the results obtained by doctors.56,57
In countries with limited resources, effective and inexpensive braces can be made using local systems. Ponseti programs have been initiated in many developing countries, including Uganda, Nepal, India and Ecuador, with the ultimate goal of providing access to Ponseti treatment for all children in the world born with clubfoot.4,93–97
However, many challenges remain, including sustainable financing, access to care, long travel distances, staff training, performing a safe tenotomy, and access to quality, affordable corsets.98 A chain of Value Care recommends the following 6 steps for optimal program success: early diagnosis, development of high volume Ponseti centers, training of non-medical health workers, involving families in care, addressing access barriers, and provide follow-up in the patient’s community.99
| Conclusions and future directions |
Treatment of idiopathic congenital clubfoot with the Ponseti method is now accepted as superior to other methods in the United States and the world.
The Ponseti method is effective, but needs to be followed closely by trained doctors and surgeons. The importance of parents adhering to the entire stabilization program cannot be overstated. A positive communication style between parents and pediatrician can improve bracing adherence and treatment success. Ponseti treatment programs are now available in many countries with limited resources. In the future, the goal of every child in the world born with a clubfoot having access to care with the Ponseti method will become a reality.
| Comment |
This work highlights the importance of knowing the Ponseti method for the treatment of clubfoot. It is the most effective, accepted treatment with low relapse rates. It is emphasized that the success of the treatment depends on a correct understanding and commitment of the parents to carry out the stabilization phase adequately and in a sustained manner over time.
On the other hand, it is a treatment that can be carried out in countries with limited resources, adapting the method to the available resources.
The final long-term objective is to ensure that every child born with idiopathic congenital botfoot has access to the Ponseti method to achieve a deformity-free, functional and comfortable foot to avoid long-term consequences and inequalities in social and labor access.















