It is well understood that sex and gender interplay with various factors such as race, ethnicity, socioeconomic status, disability, age, and sexual orientation to influence human health. Sex pertains to biological aspects tied to physical and physiological characteristics like hormones, sex chromosomes, and reproductive anatomy. In contrast, gender refers to the socially constructed roles, behaviors, and identities of women, men, and gender-diverse individuals, shaped by historical and cultural contexts. These interconnected biological and social processes lead to different health and illness experiences for men, women, and individuals of diverse sexual and gender identities.
Existing research shows that women, despite experiencing a higher prevalence of non-fatal illnesses, including chronic diseases, tend to live longer than men across nearly all global contexts. This phenomenon is known as the survival paradox between men and women. In this analysis, we utilize available data to examine health differences between women and men, as there is limited data on health outcomes for other sexual categorizations (such as intersexuality) and gender identities.
Background
Sex and gender influence health outcomes. Increasing evidence systematically examines the extent, persistence, and nature of health differences between women and men. Our objective was to quantify the differences in the leading causes of disease burden between women and men across various ages and regions.
Methods
Using data from the 2021 Global Burden of Disease Study, we compared disability-adjusted life years (DALYs) rates for women and men for the top 20 causes of disease burden in individuals aged 10 and older, both globally and across seven world regions, from 1990 to 2021. We present both absolute and relative differences in cause-specific DALY rates between women and men.
Results
Globally, women experienced a higher disease burden driven by morbidity, with the largest differences in disability-adjusted life years (DALYs) rates observed for lower back pain (478.5 [95% uncertainty interval: 346.3–632.8] more DALYs per 100,000 people among women than men), depressive disorders (348.3 [241.3–471.0]), and headache disorders (332.9 [48.3–731.9]).
In contrast, men had higher DALY rates for conditions driven by mortality, with the largest differences in DALYs observed for COVID-19 (1767.8 [1581.1–1943.5] more DALYs per 100,000 among men than women), road injuries (1012.2 [934.1–1092.9]), and ischemic heart disease (1611.8 [1405.0–1856.3]).
Sex differences increased with age and remained consistent over time for all diseases except HIV/AIDS. The greatest difference in HIV/AIDS burden was seen in individuals aged 25 to 49 in sub-Saharan Africa, with 1724.8 (918.8–2613.7) more DALYs per 100,000 among women than men.
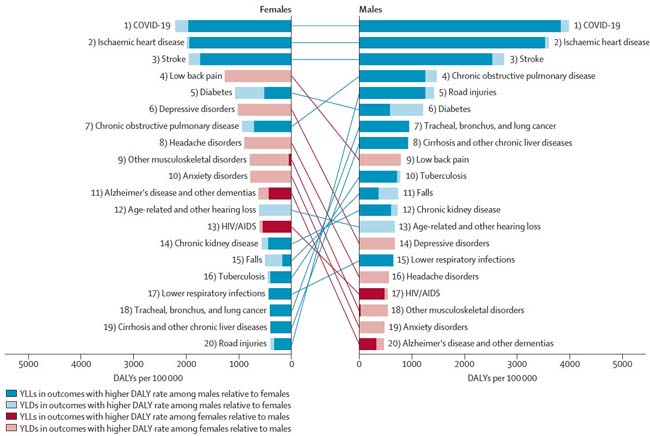
Figure: Global Rankings of the Top 20 Causes of DALYs Worldwide for Women and Men, Age-Standardized (10 Years and Older), 2021
The significant health differences between women and men highlight the urgent need for policies based on sex- and age-specific data. Additionally, it is crucial to continue promoting gender-sensitive research and ultimately implement interventions that not only reduce the disease burden but also achieve greater health equity.
Added Value of This Study
This study systematically explores health differences between women and men according to the main causes of disease burden. We used data from GBD 2021 to analyze global and regional patterns in health loss among women and men across different age groups and years for the top 20 causes of disease burden.
Disability-adjusted life years (DALYs) for mental, musculoskeletal, and neurological disorders were higher globally for women, while DALY rates for COVID-19, road injuries, ischemic heart disease, stroke, liver diseases, and tuberculosis were higher for men. In several conditions, differences between women and men emerged at an early age and continued to grow throughout life.
Moreover, our findings highlight various regional patterns in the distribution of disease burden across age groups for women and men. Providing similar estimates on conditions, regions, and time enables researchers and policymakers to clearly identify key health differences and inform priority areas for interventions aimed at addressing disparities in health outcomes between women and men.
Implications of All Available Evidence
Our research reveals substantial global health differences between women and men, with minimal progress in reducing these disparities from 1990 to 2021. Many conditions that disproportionately affect women or men, such as depressive disorders, anxiety disorders, and road injuries, start to diverge in adolescence. Existing research suggests that this period coincides with a critical age when gender norms and attitudes intensify, and puberty reshapes self-perceptions. Collectively, this evidence underscores the importance of developing gender-sensitive interventions and preventive measures from an early age.
Health disparities continue to widen with age, resulting in significant health differences between women and men at all life stages. While the empirical basis for these differences is growing, the increasing proportion of aging women and men in populations highlights the need for researchers and policymakers to recognize that women´s healthcare needs extend beyond traditionally prioritized areas such as reproductive health services.
Our analysis, along with other studies, identified significant geographical variations in the trends of health differences between women and men. These patterns emphasize the complex, context-specific relationships between health and gender norms, economic conditions, and social practices, necessitating more granular analyses to provide deeper contextual insights into the underlying factors driving health disparities. Furthermore, our analysis contributes to the current global health movement advocating for inclusive health data that incorporates sex and gender information at both the data collection and reporting stages.
Discussion
Based on estimates from the GBD 2021, we identified persistent health differences between women and men in the 20 leading causes of disease burden over the past three decades. In 2021, men generally faced a greater disease burden than women. For 13 of the top 20 causes, including COVID-19, road injuries, and various cardiovascular, respiratory, and liver diseases, men had higher DALY rates than women. Women had higher age-standardized DALY rates associated with lower back pain, depressive disorders, headaches, anxiety, other musculoskeletal disorders, Alzheimer´s disease and other dementias, and HIV/AIDS than men. These differences underscore the importance of addressing the distinct health needs of women and men throughout their lives.
Historically, attention to women´s health has largely focused on sexual and reproductive issues which, although crucial, do not cover the full spectrum of health problems affecting women over their lifetimes. Our analysis highlights, for example, the disproportionate burden of morbidity-driven conditions among women, with the largest differences seen in mental and musculoskeletal disorders. Non-communicable diseases that more commonly affect women remain underprioritized in research funding, scientific literature, and notably in health system planning, both in terms of trained professionals and allocated funding, despite the associated health and economic burden. For instance, the WHO´s 2020 Mental Health Atlas highlights the global shortage of health workers trained in mental health, especially in low- and middle-income countries (LMICs), where the rate of mental health workers can be as low as two per 100,000 people, compared to over 60 in high-income countries. Additionally, the report reveals that globally, only 2.1% of public health spending is directed towards mental health, which is particularly concerning given the enormous burden of mental health disorders that disproportionately affect women across regions.
Notably, the health differences we identified begin at an early age, a stage marked by pubertal changes and intensified gender socialization, when gender identity, roles, and norms diverge significantly and gain prominence—emphasizing the need for early, targeted responses. Moreover, differences between women and men continue to grow with age in many diseases, leaving women with higher degrees of morbidity over their lifetimes, which are on average longer than those of men.
Aging populations worldwide place greater demands on already overburdened healthcare systems, necessitating increased funding and stronger infrastructure to meet the changing needs of their populations. The higher degree of morbidity among women, combined with the increasing proportion of aging women and men, are crucial components that policymakers must consider when preparing their health systems for the coming decades. This is particularly important for LMICs, where the shift in the age structure of populations occurs alongside ongoing challenges with infectious diseases.
Funding
This study was funded by the Bill and Melinda Gates Foundation.
















