Summary Aim Undiagnosed or inadequately treated dry eye disease (DED) decreases quality of life. Our objective was to investigate the reliability, validity, and feasibility of the DryEyeRhythm smartphone application (app) for DED diagnosis assistance. Methods This prospective, cross-sectional, observational, single-center study recruited 82 participants (42 with DED) aged 20 years or older (July 2020 to May 2021). Patients with a history of eyelid disorder, ptosis, mental illness, Parkinson’s disease, or any other disease affecting blinking were excluded. Participants underwent DED examinations including the Japanese version of the Ocular Surface Disease Index (J-OSDI) and maximum blink interval (MBI). We analyze your application-based J-OSDI and MBI results. Internal consistency reliability and concurrent validity were assessed using Cronbach’s alpha coefficients and Pearson’s test, respectively. The discriminant validity of the application-based DED diagnosis was assessed by comparing the results of the clinic-based J-OSDI and the MBI. The application feasibility and detection performance were evaluated by analyzing the receiver operating characteristic curve and accuracy rate. Results The application-based J-OSDI showed good internal consistency (Cronbach’s α = 0.874). The app-based J-OSDI and MBI were positively correlated with their clinical counterparts (r = 0.891 and r = 0.329, respectively). Discriminant validity of the app-based J-OSDI and MBI produced significantly higher total scores for the DED cohort (8.6 ± 9.3 vs. 28.4 ± 14.9, P < 0.001, 19.0 ± 11.1 vs. 13.2 ± 9.3, P < 0.001). The positive and negative predictive values of the application were 91.3% and 69.1%, respectively. The area under the curve (95% confidence interval) was 0.910 (0.846–0.973) with simultaneous use of application-based J-OSDI and MBI. Conclusions The DryEyeRhythm application is a novel, non-invasive, reliable and valid instrument for evaluating DED. |
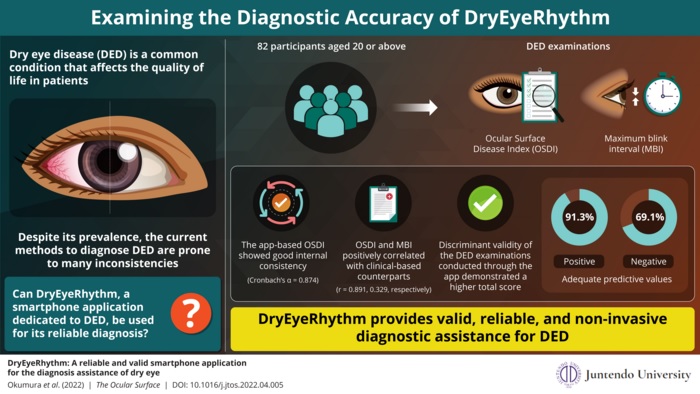
Image : The results show that DryEyeRhythm diagnostic results have good internal consistency, positively correlate with their clinical counterparts, and demonstrate greater discriminant validity. Credit: Juntendo University
Comments
Dry eye disease (DED) is a condition characterized by a variety of different symptoms, including dryness, eye discomfort, fatigue, and visual disturbances. This condition has become increasingly common in recent years due to an aging society, increased screen time, and a highly stressful social environment. There are about 1 billion people worldwide who have DED. Undiagnosed and untreated DED can cause a variety of symptoms, including eye fatigue, light sensitivity, reduced quality of vision, and a lower quality of life. Given the widespread prevalence of the condition, this can further lead to reduced work productivity and economic losses.
Despite the obvious disadvantages of DED, a large portion of the population remains undiagnosed, ultimately leading to increased disease severity. Currently, DED is diagnosed through a series of questionnaires and eye exams (which can be invasive). But this diagnostic method is not ideal. DED examinations do not always correspond to patients’ subjective DED symptoms. Additionally, non-invasive and non-contact dry eye examinations are required in the COVID-19 pandemic. These shortcomings point to the need for a simple, reliable, and accessible screening method for DED to improve the diagnosis and prognosis of the disease.
To respond to this need, a research group, led by Professor Akira Murakami and Associate Professor Takenori Inomata from Juntendo University School of Medicine, developed a smartphone application called DryEyeRhythm. “DryEyeRhythm leverages smartphone cameras to measure users’ blinking characteristics and determine maximum blink interval (MBI), a surrogate for tear film breakup time, an important diagnostic criterion for DED. ” explains Associate Professor Inomata. “The app also administers Ocular Surface Disease Index (OSDI) questionnaires, which are also a crucial component of DED diagnosis.”