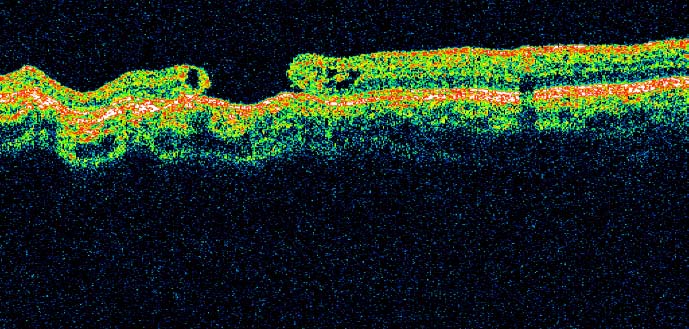
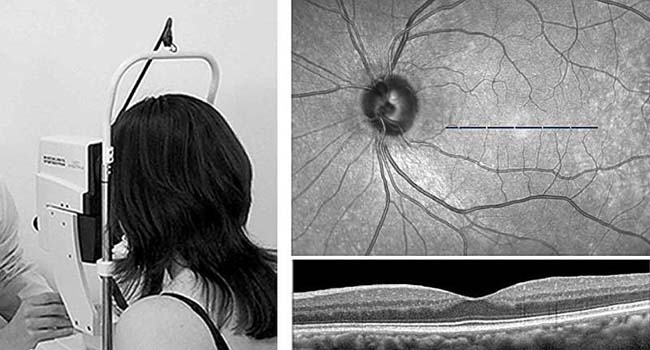
Optical coherence tomography (OCT) has become a valuable tool for evaluating retinal changes associated with neurodegenerative diseases, including Parkinson´s disease (PD). OCT allows high-resolution, reproducible and accurate measurements of retinal layer thickness to detect structural alterations. Among retinal layers, the ganglion cell inner plexiform layer (GCIPL) has attracted substantial attention due to its potential as a biomarker of neurodegeneration and cognitive decline.
Optical coherence tomography. LaNCE-Neuropharm—GIC 21/133
Association of retinal neurodegeneration with the progression of cognitive impairment in Parkinson´s disease
Summary
Retinal thickness may serve as a biomarker in Parkinson´s disease (PD). In this prospective longitudinal study, we aimed to determine whether PD patients have an accelerated rate of thinning in the parafoveal ganglion cell inner plexiform layer (pfGCIPL) and peripapillary retinal nerve fiber layer (pRNFL) compared to controls. Furthermore, we evaluated the relationship between retinal neurodegeneration and clinical progression in PD.
A cohort of 156 PD patients and 72 controls underwent retinal optical coherence tomography and visual and cognitive assessments between February 2015 and December 2021 at two Spanish tertiary hospitals. The pfGCIPL thinning rate was twice as high in PD (β [SE] = −0.58 [0.06]) than in controls (β [SE] = −0.29 [0.06], p < 0.001). In PD, the pattern of progression of pfGCIPL atrophy was dependent on initial thickness, with slower thinning rates observed in PD patients with pfGCIPL below 89.8 µm. This result was validated using an external dataset from Moorfields Eye Hospital NHS Foundation Trust (AlzEye study). Slow pfGCIPL progressors, characterized by older baseline age, longer disease duration, and worse cognitive and disease stage scores, showed a three-fold increase in the rate of cognitive decline (β [SE] = − 0.45 [0.19] points/year, p = 0.021) compared to faster progressors. Furthermore, thinning of the pRNFL of the temporal sector was accelerated in PD (β time × group [SE] = −0.67 [0.26] μm/year, p = 0.009), demonstrating a close association with the changes in the cognitive score (β [SE] = 0.11 [0.05], p = 0.052).
This study suggests that a slower pattern of pfGCIPL tissue loss in PD is related to more rapid cognitive decline, while changes in temporal pRNFL could follow cognitive decline.
Comments
Although there are still some aspects to be confirmed for its use in the clinical setting, and its resolution needs to be slightly improved, a study by the UPV/EHU and Biobizkaia has shown that a method commonly used to perform ophthalmological tests can also be used to monitor the neurodegeneration that occurs in Parkinson´s patients .
During the research it was discovered that retinal neurodegeneration probably precedes cognitive decline.
When Parkinson´s or another neurodegenerative disease is diagnosed, patients always ask: "What now? What will happen? What can be expected from the disease?" For neurologists, however, it is not possible to answer these questions precisely, since "the evolution of patients is usually very varied: some do not experience changes over the years, while others end up with dementia or in a chair." wheels," explains Ane Murueta. -Goyena, researcher at the Department of Neurosciences at the UPV/EHU.
Today, identifying Parkinson´s patients at risk of cognitive impairment is very challenging, but necessary when it comes to providing more effective clinical treatments and intensifying clinical trials.
In fact, Dr. Ane Murueta-Goyena, in collaboration with the Biobizkaia research staff, wanted to check "if the visual system can predict this deterioration, that is, what future awaits the patient in a few years." For this, the thickness of the retina was used.
The retina is a membrane located at the back of the eyeball; It is related to the nervous system and comprises several layers. During the study, the thickness of the innermost layer of the retina of a cohort of Parkinson´s patients was measured using optical coherence tomography.
This type of tomography is an instrument commonly used in ophthalmological tests, since it allows high-resolution, repeatable and precise measurements to be made. Thus, the evolution of this retinal layer was analyzed and compared in people with and without Parkinson´s disease during the period 2015-2021. The results of the analysis of images of the retinal layers of Parkinson´s patients were also confirmed in a hospital in the United Kingdom.
The results showed that the retinal layer is noticeably thinner in Parkinson´s patients. It was also observed that "during the initial phases of the disease, it is in the retina where the greatest neurodegeneration is detected , and, from a given moment, when the layer is already very thin, a kind of stabilization of the neurodegeneration process occurs. ".
"Retinal thinning and cognitive impairment do not occur simultaneously. The initial changes in the retina are more evident and then, as the years go by, patients are observed to worsen clinically both in cognitive and motor terms," Murueta explained. -Goya. "In other words, slower loss of retinal layer thickness is associated with faster cognitive decline; this slowness is related to greater disease severity."
The researcher has attached great importance to the results. "We have obtained information about the progression of the disease and the tool we propose is non-invasive and available in all hospitals."
The results need to be validated internationally and "by slightly improving the resolution of the technology, we will be closer to validating the method for monitoring the neurodegeneration that occurs in Parkinson´s disease." The researcher also revealed that they continue the research in another cohort of patients and that financing is the key.
Discussion
This longitudinal cohort study revealed that the rate of retinal thinning was significantly higher in PD patients compared to controls, particularly in pfGCIPL and the temporal sector of pRNFL. Our findings indicate that the rate of retinal neurodegeneration varies among people with PD. Specifically, PD patients with greater baseline pfGCIPL atrophy showed slower rates of pfGCIPL thinning over time. These individuals had longer disease duration and greater disease severity, as assessed by cognitive assessments (MoCA) and motor assessments (H&Y scale). Interestingly, in this group of severe PD patients with baseline retinal atrophy and slower pfGCIPL thinning, cognitive decline progressed significantly faster than in other PD patients. This finding highlights an uncoupled progression between macular changes and cognitive decline, suggesting that macular neurodegeneration may precede cognitive decline.
Therefore, we interpret that once a certain threshold of retinal macular atrophy is reached, there is a potential slowdown in its degeneration pattern. This slowdown reflects greater disease severity , which is accompanied by an acceleration of the progression of cognitive decline. In contrast, thinning in the temporal sector of pRNFL showed a close association with alterations in MoCA score, suggesting a simultaneous progression that could serve as a valuable indicator for monitoring cognitive decline.
Reference: Ane Murueta-Goyena et al, Association of retinal neurodegeneration with the progression of cognitive decline in Parkinson´s disease , npj Parkinson´s Disease (2024). DOI: 10.1038/s41531-024-00637-x