Disruption of the blood-brain barrier and sustained systemic inflammation in people with long-term cognitive impairment associated with COVID Summary Vascular disruption has been implicated in the pathogenesis of coronavirus disease 2019 (COVID-19) and may predispose to neurological sequelae associated with long COVID, but it is unclear how blood- brain barrier (BBB) function is affected. in these conditions. Here we show that BBB disruption is evident during acute infection and in long COVID patients with cognitive impairment, commonly known as confusion or brain fog . Using dynamic contrast-enhanced magnetic resonance imaging, we show BBB disruption in patients with long-term COVID-associated mental confusion. Transcriptomic analysis of peripheral blood mononuclear cells revealed dysregulation of the coagulation system and an attenuated adaptive immune response in individuals with mental confusion. Accordingly, peripheral blood mononuclear cells showed increased adhesion to human brain endothelial cells in vitro , while exposure of brain endothelial cells to serum from long COVID patients induced the expression of inflammatory markers. Taken together, our data suggest that sustained systemic inflammation and persistent localized BBB dysfunction are a key feature of long-term mental confusion associated with COVID . |
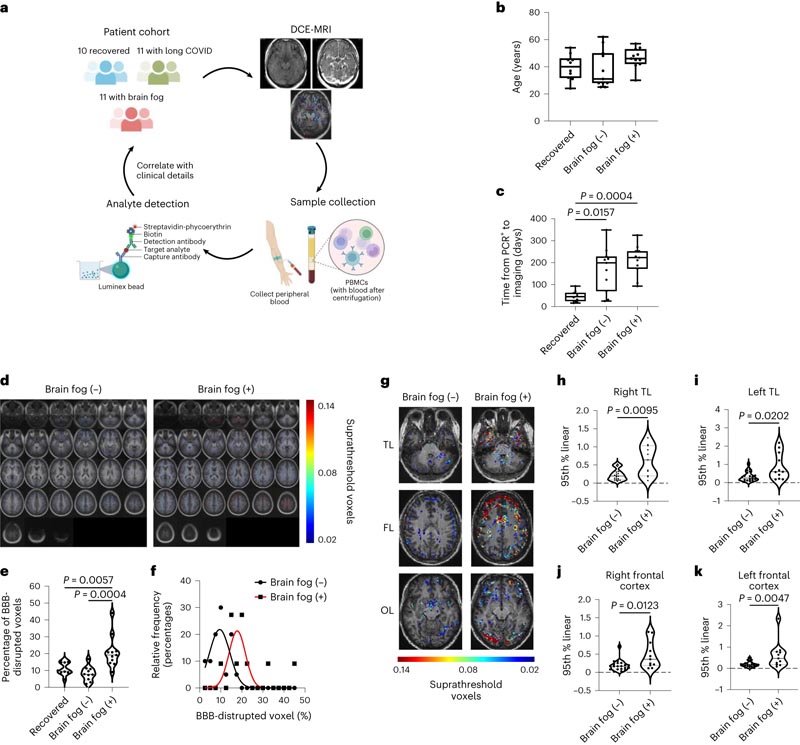
Figure: a, Patient cohort for dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI). b, Age distribution between cohorts ( n = 10 recovered, n = 11 without mental confusion (-), n = 11 with mental confusion (+)). c, Time from COVID + PCR test to scan in all cohorts ( n = 10 recovered, n = 11 without mental confusion (-), n = 11 with mental confusion (+)). Data were analyzed using a two-sided Kruskal-Wallis test with Dunn’s correction for multiple comparisons ( P = 0.0157 without mental confusion (-) versus recovered; P = 0.0004 with mental confusion (+) versus recovered). d, BBB permeability maps averaged in cases with and without mental confusion. e, Quantification of the percentage of brain volume with leaky blood vessels in the mental confusion cohort compared with recovered cases ( P = 0.0057) and non-mental confusion cases ( P = 0.0004). Data were analyzed using one-way analysis of variance with Tukey’s correction. f, Frequency distribution of the percentage of voxels altered by BBB in cases with and without mental confusion. g , Representative maps of BBB permeability at the level of TL, FL, and OL showing increased BBB permeability in cases with mental confusion. h–k, Quantification of regional BBB permeability in the right TL (P = 0.0095) (h), the left TL (P = 0.0202) (i), the right frontal cortex (P = 0.0202) (i), 0123) (j) and the left frontal cortex (P = 0.0047) (k). Data were analyzed using a two-sided Mann-Whitney U test. Boxplots show the minimum and maximum values (whiskers), median (solid line), and interquartile range (IQR) (upper and lower box). The violin plots show the median (solid line) and IQR (dashed lines); each data point represents one patient. The schematics in a were created with BioRender.com
Comments
Researchers discover link between leaky blood vessels in brain and long Covid patients reporting mental confusion
A team of scientists from Trinity College Dublin and researchers from FutureNeuro announced a major discovery that has profound significance for our understanding of the brain fog and cognitive impairment seen in some long COVID patients.
In the months following the emergence of the novel coronavirus SARS-CoV2 in late 2019, a patient-reported syndrome called long COVID began to come to the fore as a long-lasting manifestation of an acute infection.
To date, long COVID has up to 200 reported symptoms, but generally patients report persistent symptoms such as fatigue, shortness of breath, problems with memory and thinking, and joint/muscle pain . While the vast majority of people who suffer from COVID-19 make a full recovery, any of these symptoms that persist for more than 12 weeks after infection can be considered long COVID.
Long COVID has become a major public health problem since the outbreak of the pandemic in 2020. While international incidence rates vary, it is estimated to affect up to 10% of patients infected with the SARS-CoV2 virus. Of these long COVID patients, just under 50% report some type of lingering neurological effect, such as cognitive impairment, fatigue, and brain fog .
Now, findings reported by the Trinity team in the leading international journal Nature Neuroscience showed that there was an alteration in the integrity of blood vessels in the brain of patients suffering from long COVID and mental confusion. This “leak” from the blood vessels was able to objectively distinguish patients with brain fog and cognitive impairment compared to patients who had long COVID but not brain fog.
The team led by scientists from the Smurfit Institute of Genetics in Trinity’s School of Genetics and Microbiology and neurologists from the School of Medicine have also discovered a new form of MRI scan that shows how long COVID can affect the delicate network of vessels blood vessels of the human brain.
“For the first time, we have been able to show that leaky blood vessels in the human brain, along with an overactive immune system , may be key drivers of the brain fog associated with long COVID. This is vitally important as understanding the underlying cause of these conditions will allow us to develop targeted therapies for patients in the future,” said Prof Matthew Campbell, Professor of Genetics and Head of Genetics at Trinity, and Principal Investigator of FutureNeuro.
This project was initiated by a rapid response grant funded by Science Foundation Ireland (SFI) at the height of the pandemic in 2020 and involved the recruitment of patients suffering from the effects of Long-COVID, as well as patients hospitalized in St James’ Hospital.
“Conducting this complicated clinical research study at a time of national crisis and when our hospital system was under great pressure is a testament to the skill and resources of our medical staff and students. The findings are now likely to change the landscape of how we understand and treat post-viral neurological conditions . “It also confirms that the neurological symptoms of Long Covid can be measured by real, demonstrable metabolic and vascular changes in the brain,” said Prof. Colin Doherty, Professor of Neurology and Head of Trinity School of Medicine, and Principal Investigator of FutureNeuro. .
Beyond COVID-19
In recent years, it has become evident that many neurological conditions, such as multiple sclerosis (MS), likely have a viral infection as the initial event that triggers the pathology. However, proving that direct link has always been a challenge.
Professor Campbell added: “Here, the Trinity team was able to demonstrate that every patient who developed Long-COVID had been diagnosed with SARS-CoV2 infection, because Ireland required every documented case to be diagnosed using more accurate PCR-based methods. . “The concept that many other viral infections leading to post-viral syndromes could cause leaky blood vessels in the brain is potentially a game-changer and the team is actively investigating it.”
Dr Chris Greene, postdoctoral researcher and first author of the study, added: “Our findings have now laid the foundation for future studies examining the molecular events that lead to post-viral fatigue and brain fog . "There are certainly similar mechanisms at play in many different types of viral infections and we are now very close to understanding how and why they cause neurological dysfunction in patients."
















