Cognitive symptoms after COVID-19, caused by the SARS-CoV-2 virus, are well recognized. However, it´s still uncertain whether there are objectively measurable cognitive deficits and for how long they last.
In a study conducted in England, 800,000 adults were invited to complete an online cognitive function assessment. Cognitive performance was evaluated through eight tasks, and it was hypothesized that participants with persistent symptoms (lasting ≥12 weeks) post-infection would show global cognitive deficits, particularly in executive functioning and memory. This was expected to be especially noticeable in those reporting poor recent memory or difficulty concentrating (often referred to as "brain fog").
Out of 141,583 participants who began the cognitive assessment, 112,964 completed it.
In a multiple regression analysis, those who had recovered from COVID-19 with resolved symptoms (either in less than 4 weeks or after at least 12 weeks) showed small but similar deficits in global cognition compared to a non-COVID-19 group (which had no confirmed infection) with cognitive scores slightly reduced by -0.23 SD [95% confidence interval {CI}, -0.33 to -0.13] and -0.24 SD [95% CI, -0.36 to -0.12]. More significant deficits were observed in those with unresolved persistent symptoms (-0.42 SD; 95% CI, -0.53 to -0.31).
Larger deficits were found in participants who had contracted SARS-CoV-2 when the original virus or the B.1.1.7 variant was dominant, compared to those infected with later variants (e.g., -0.17 SD for B.1.1.7 compared to the B.1.1.529 variant; 95% CI, -0.20 to -0.13). Participants who had been hospitalized, particularly those admitted to intensive care, experienced more significant cognitive deficits (e.g., -0.35 SD for ICU admission; 95% CI, -0.49 to -0.20).
The results were similar when analyzed using propensity score matching. In a comparison of those with unresolved persistent symptoms and the non-COVID-19 group, the greatest deficits were seen in memory, reasoning, and executive function tasks (-0.33 to -0.20 SD). These cognitive deficits were weakly correlated with recent symptoms like poor memory and mental confusion.
No adverse events were reported.
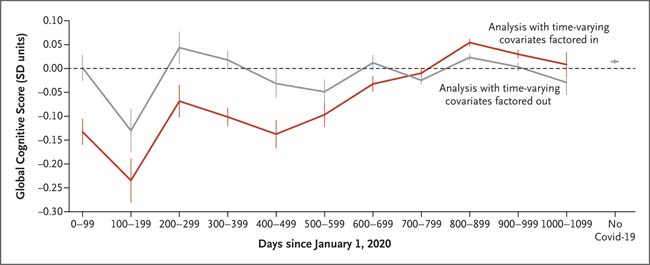
Figure: Cognitive Function Over Time
The figure illustrates the association between global cognitive scores and infection date among 58,108 participants who had a single SARS-CoV-2 infection. The red line represents scores before adjusting for covariates (such as disease duration, hospitalization, and virus variant) while the gray line shows the results after adjusting for these factors. Non-COVID-19 participants’ results appear on the right side of the graph. The error bars represent the 95% confidence intervals.
Participants who had resolved persistent symptoms displayed cognitive function comparable to those with shorter-lasting symptoms, though even short-duration COVID-19 was linked to minor cognitive deficits post-recovery. The long-term persistence of these cognitive deficits and their clinical implications remain uncertain.
In this observational study, we found that objectively measurable cognitive deficits can persist for a year or more after COVID-19. Those with resolved persistent symptoms had small cognitive deficits compared to non-COVID-19 participants, similar to those with shorter illnesses.
Early pandemic periods, prolonged illness duration, and hospitalization were most strongly associated with global cognitive deficits. The long-term relevance of these deficits and their clinical impact remain unclear and warrant further monitoring.
















