The long-term effects of COVID-19 on cognitive function have become an area of growing concern. This article provides an overview of the characteristics, risk factors, possible mechanisms and management strategies of cognitive dysfunction in the post-COVID-19 condition (PCC).
Prolonged cognitive dysfunction is one of the most common impairments in the post-COVID-19 condition (PCC), affecting between 17% and 28% of individuals more than 12 weeks after infection and persisting in some cases for several years.
Cognitive dysfunctions can manifest as a wide range of symptoms including memory impairment, attention deficits, executive dysfunction, and reduced processing speed .
Risk factors for developing PCC, with or without cognitive impairment, include advanced age, preexisting medical conditions, and severity of acute illness. The underlying mechanisms remain unclear, but proposed contributors include neuroinflammation, hypoxia, vascular damage, and reactivation of latent virus, without excluding the possibility of direct viral invasion of the central nervous system, illustrating a complex viral pathology.
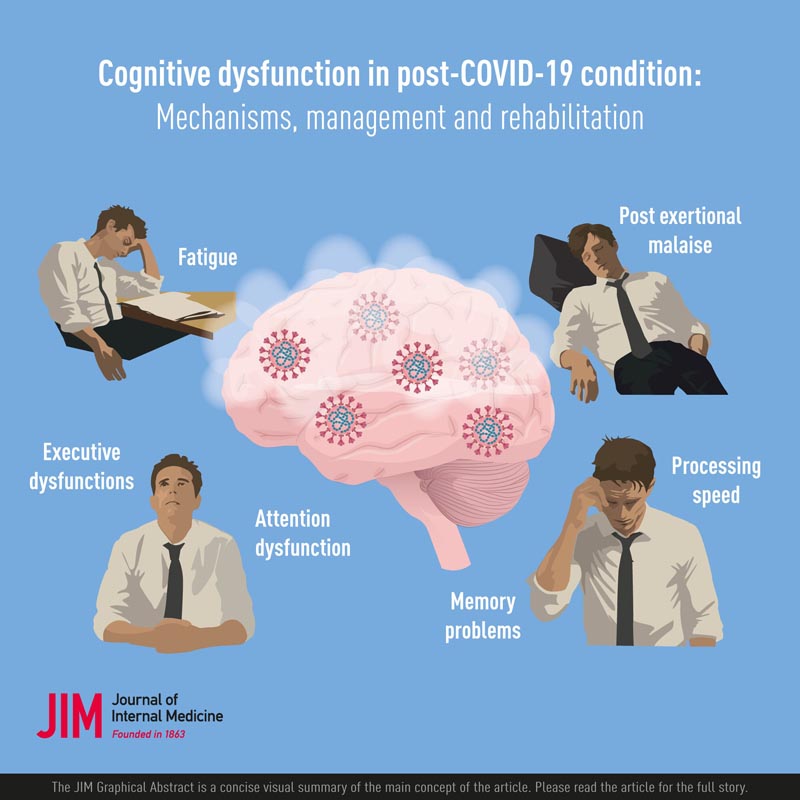
Cognitive symptoms
Attention functions allow the ability to process information from our environment and are considered hierarchical in nature. Focused attention and sustained attention are considered fundamental attentional functions. Higher levels of attention depend on executive functions and encompass alternating, selective, and divided attention. Despite its name, working memory is also considered a function of attention and plays an important role in memory encoding and retrieval of information stored in long-term memory.
Since attention functions serve as fundamental cognitive processes and subsystems for other cognitive functions, they are crucial for managing our daily lives. Impaired attention functions, even in cases of mild impairments, directly affect performance in both daily tasks and work life.
Attention functions are frequently associated with processing speed. From a neuroanatomical perspective, the thalamus plays a crucial role as a hub for networks that support processes related to attention, information processing, memory, and executive functions. However, the studies carried out to date on COVID-19 have not determined which of the attention functions is most affected in PCC, nor to what extent other cognitive dysfunctions are independent or linked to diminished attention functions. .
Impairments in attention, working memory, and executive functions often have side effects on tests that assess memory encoding and retrieval. Consequently, episodic memory may be indirectly affected by the type of neurological damage caused by viral diseases, primarily through reductions in attention and processing speed necessary for encoding. In the context of PCC, it is not yet fully established whether the results observed in memory tests are due to primary difficulties in memory storage or whether they are secondary effects resulting from an impairment of attention and/or memory of job.
Fatigue
Fatigue is a prominent symptom in both acute COVID-19 and PCC. Prevalence rates of post-COVID fatigue range between 32% and 46% in different studies and in the meta-analysis of 1-year follow-ups between 18% and 39%. However, fatigue is a multifactorial and vaguely defined symptom present in various conditions, including neurological disorders, chronic pain, and depression. Post-infectious fatigue has also been reported after other viral epidemics.
In most studies, fatigue is reported subjectively using self-rating scales designed to capture a low level of energy that is not proportional to the individual’s activity level and is not relieved by normal rest or sleep. Currently, there is no validated fatigue scale specifically for post-COVID fatigue.
As COVID-19 is a new condition, it is not evident whether the fatigue experienced in PCC is equivalent and shares the same underlying mechanisms as fatigue in neurological conditions. In neurological conditions, decreased attention, decreased processing speed, and fatiguability have been linked to the experience of fatigue, but have also shown significant correlations with depression and sleep disorders.
Approach
As individual variation in cognitive impairments is large, neuropsychological examination and a multidimensional person-centered approach are required. According to the World Health Organization, limited evidence on cognitive impairments related to COVID-19 requires the implementation of rehabilitation interventions based on established practices for similar conditions.
Psychoeducation and training in compensatory skills is recommended. Assistive products and environmental modifications tailored to individual needs may be helpful.
In specific dysfunctions of attention and working memory, cognitive training (carefully controlled in terms of intensity) could be effective for people who do not suffer from post-exertional malaise.
Further research is crucial for evidence-based interventions specific to COVID-19-related cognitive impairments.
Conclusions Prolonged cognitive dysfunction is a common impairment affecting people with PCC. Risk factors for PCC generally include female sex, age, preexisting medical conditions, and severity of acute illness. Proposed mechanisms contributing to PCC and cognitive impairments include neuroinflammation, hypoxia, vascular damage, latent viral reactivation, and direct viral invasion of the central nervous system. Management of cognitive dysfunction in PCC requires a multidimensional approach that includes neuropsychological examination and individualized rehabilitation. Although evidence specific to COVID-19-related cognitive impairments is limited, interventions can be implemented based on established practices for other neurological conditions. The WHO recommends education, skills training, cognitive exercises, assistive products and environmental modifications. Functional training with careful control of intensity is recommended for people who do not suffer from PEM. Further research is essential for evidence-based interventions specific to COVID-19-related cognitive impairments. |
















