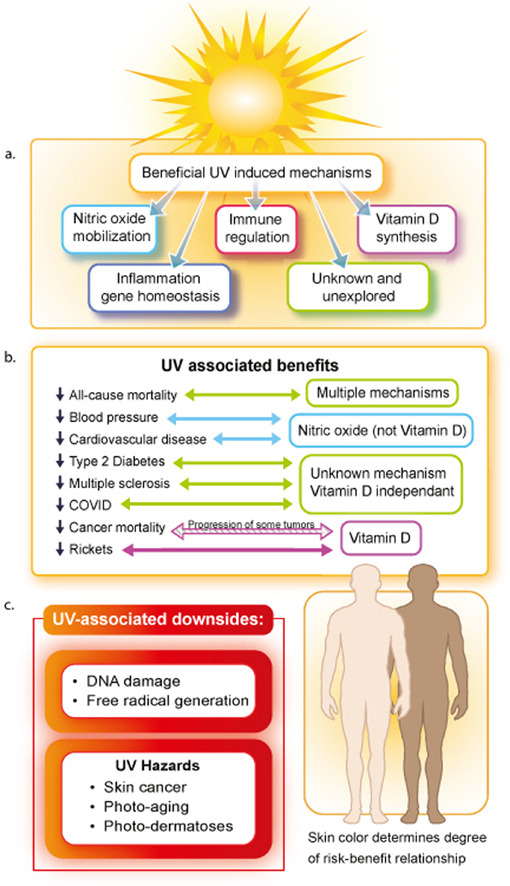
This article proposes a reassessment of the current understanding of sunlight exposure and its effects on health, urging medical professionals to consider both the risks and systemic benefits when formulating public health recommendations. While UV radiation is a well-established carcinogen for the skin, emerging evidence highlights significant systemic benefits that should not be overlooked.
Key Points for Consideration:
No Evidence of Increased All-Cause Mortality
Despite the established link between UV radiation and skin cancer, there is no evidence to suggest that sunlight exposure increases all-cause mortality. This underscores the need to balance skin cancer risks with broader health outcomes.Epidemiological Evidence Supporting Sunlight Benefits
Studies from the UK and Sweden have demonstrated an association between sunlight exposure and reduced all-cause mortality, including lower rates of cardiovascular diseases and certain cancers. These findings suggest that sunlight may have protective effects beyond its role in vitamin D synthesis.Vitamin D-Independent Pathways
Sunlight exposure activates pathways independent of vitamin D, such as the photomobilization of nitric oxide (NO) from the skin. This mechanism contributes to reduced blood pressure and improved cardiovascular health, highlighting the multifaceted benefits of UV exposure.Evolutionary Insights into Skin Pigmentation
The evolutionary selection of fair skin in higher latitudes is often attributed to the need for efficient vitamin D synthesis in low-UV environments. However, other factors, such as reduced susceptibility to infectious diseases, may also have influenced this adaptation.Nitric Oxide and Cardiovascular Health
Exposure to UVA and UVB radiation mobilizes NO from the skin, leading to vasodilation, reduced blood pressure, and lower cardiovascular morbidity. This pathway represents a critical link between sunlight exposure and systemic health benefits.Additional Mechanisms of Action
Beyond NO mobilization, sunlight exposure may modulate immune function through mechanisms such as cis-urocanic acid production and influence gene expression. These effects warrant further investigation to fully understand their clinical implications.Myopia and Reduced Outdoor Time
The rising global incidence of myopia has been linked to decreased time spent outdoors. This association suggests that sunlight exposure may play a protective role in eye health, challenging current recommendations that emphasize sun avoidance.The "Sunlight Quartet": Diseases Associated with Sunlight Deficiency
The article introduces the concept of the "sunlight quartet," which identifies conditions that may benefit from UV exposure, including multiple sclerosis, hypertension, type 2 diabetes, and COVID-19. These associations highlight the potential public health impact of sunlight deficiency.The Role of Skin Color in Risk-Benefit Assessment
Skin pigmentation significantly influences the biological response to UV radiation. Medical professionals must consider individual skin color when assessing the risks and benefits of sunlight exposure to provide personalized recommendations.
Conclusion: A Call for a Broader Perspective
The medical community, particularly dermatologists, should adopt a more comprehensive view of sunlight exposure that integrates both its risks and systemic health benefits. While skin cancer prevention remains a priority, the potential benefits of sunlight for cardiovascular health, immune function, and other systemic conditions cannot be ignored. Further research is essential to elucidate the mechanisms underlying these effects and to refine public health guidelines. By embracing a balanced approach, healthcare providers can better serve their patients and promote overall health.
The relationship between sunlight and human health has been a subject of debate and evolution throughout history. While modern dermatology has focused on the risks of ultraviolet (UV) radiation to the skin, such as cancer and premature aging, there is growing evidence pointing to significant systemic benefits of sunlight exposure. This article explores these benefits and advocates for a reassessment of our perspective on sunlight, advocating for a more holistic approach that considers both the risks and health benefits.
History of UV-related skin cancer advice
Ultraviolet radiation (UVR) is an established environmental carcinogen, as confirmed by epidemiological, mechanistic, and clinical trial data. Skin cancers and melanoma are more prevalent in white-skinned populations in very sunny countries like Australia and South Africa than in the UK, although the epidemiological nature of the relationship between sunlight exposure and melanoma is less clear than for keratinocyte cancers.
Public health advice on UV exposure for much of the past century has focused on these adverse effects. Unna in 1894 first identified the link between UV exposure and skin cancer in sailors with his description of Seeman’s Haut. Findlay in 1928 provided evidence that UV rays were indeed the causative carcinogen, demonstrating that irradiating mice with a mercury vapor lamp induced epithelial neoplasms. Based on this data, the next century saw the development of better sun protection, initially through behavioral and clothing changes, and since the 1940s, a continuously evolving range of increasingly effective UV filters. Sunscreens prevent sunburn, skin aging, and squamous cell skin cancer in white-skinned people. However, there is a lack of evidence that increased sunlight exposure increases mortality from all causes or that avoiding the sun prolongs lifespan.
Epidemiological and evolutionary evidence
Homo sapiens evolved in Africa around 150,000 years ago. The divergence between our hominid ancestors and their primate ancestors involved the loss of body hair and the development of extensive sweat glands. The abundant sweat glands in hairless terminal skin allow for heat loss through evaporation, which suited the genus Homo for sustained activity necessary to hunt nutritious prey species. However, with this loss of hair, our naked epidermis became directly exposed to UV rays. Within African human populations, strict restrictions on MC1R alleles encoding eumelanin show that dark skin was the favored evolutionary adaptation to this environment.
Dispersing from Africa to low-light environments, these constraints were lost, and a series of light-skinned variants developed, not only in MC1R but also in other genes, particularly KITLG in East Asia and SLC24A5 and SLC45A2 in Europe. This repeated and independent evolution of fair skin in populations living at higher latitudes with lower ambient UV rays underscores the importance of sunlight exposure for health, though it tells us little about the mechanisms driving this evolutionary fitness gain.
From an evolutionary perspective, the selection of fair skin in populations migrating from Africa to higher latitudes has been attributed to the need to synthesize vitamin D in environments with lower UV radiation. However, recent research suggests other mechanisms, such as the reduction of infectious diseases, may have driven this adaptation.
Sunlight and mortality from all causes
Weighing the risk-benefit relationship is a central skill in medicine and is consciously or unconsciously practiced in all our interactions with patients.
When we prescribe a treatment, we consider the indication (benefit) and the side effect profile (risk). Epidemiologically, mortality from all causes represents a precise summation of the risks and benefits of any exposure and should guide public health recommendations in the same way.
Precisely quantified increases in mortality from all causes confirm the harmful effects of high blood pressure, smoking, lack of exercise, poor diet, air pollution, poverty, high cholesterol, obesity, inadequate childhood nutrition, and many other factors on health. The resulting diseases from these risk factors are varied, but all public health measures to mitigate them are based on a solid evidence base aimed at extending healthy lifespan.
There is no data linking increased mortality from all causes with sunlight exposure, despite the known carcinogenic effects of UV rays on the skin.
Surprisingly, despite the known risks to the skin, no direct relationship has been found between sunlight exposure and increased mortality from all causes. In fact, studies in the UK and Sweden suggest that increased sunlight exposure is associated with reduced mortality, including cardiovascular diseases and cancer.
Two large prospective cohort studies from northern Europe link increased sunlight exposure to reduced mortality from all causes. In the Southern Sweden Melanoma Study, 30,000 Swedish women were followed for 25 years, with sun-seeking behavior and relevant confounding factors recorded at baseline. Twenty-five years after enrollment, sun-seeking behavior was inversely correlated with mortality from all causes, despite a higher incidence of melanoma cases in those with greater sun exposure. The reduction in mortality from all causes was particularly related to lower rates of cardiovascular death.
We have analyzed the much larger UK Biobank cohort studying the relationship between sunlight exposure and mortality from all causes in around 377,000 white-skinned participants. Two independent measures of sunlight exposure (residence latitude and use of sunbeds or recliners) were used, and their accuracy as a measure of sunlight exposure was confirmed by their association with higher measured vitamin D levels. The direction of confounding factors differed for each UV exposure measure; however, in both cases, increased sunlight exposure was correlated with reduced mortality from all causes, particularly reduced cardiovascular mortality but also cancer mortality (including skin cancer).
Mortality from all causes was reduced with a hazard ratio of 0.94 (95% confidence interval = 0.92–0.96) for every 300 km further south (and hence higher sunlight exposure) after correcting for demographic, socioeconomic, behavioral, and clinical confounding factors. This equates to an increase in lifespan of 16 days per 300 km lower latitude. Data from these two independent studies confirm that, for white-skinned inhabitants of northern European countries, the benefits of sunlight exposure outweigh the risks.
Considerations on skin color
It is crucial to consider skin color when assessing the risks and benefits of sunlight exposure, as the biological response to UV radiation varies by pigmentation. People with dark skin have a lower capacity to synthesize vitamin D and release NO from the skin, which could explain differences in disease prevalence between populations.
More than just vitamin D
Epidemiological and evolutionary evidence suggests significant benefits of sunlight exposure, but it does not reveal the mechanisms. Vitamin D formation is the most studied UV-dependent biomolecule. UVB radiation is necessary for epidermal formation of cholecalciferol, the precursor to active vitamin D3, 1,25-dihydroxycholecalciferol. The measured level of vitamin D (typically individually 25-hydroxylated, hydroxycholecalciferol) serves as a useful biomarker for UVB sunlight exposure, as demonstrated by seasonal variations in vitamin D with a nadir in winter months. Calcium and phosphate metabolism depend on vitamin D, and low vitamin D levels due to inadequate diet or sunlight exposure cause rickets in children and osteomalacia in adults.
While vitamin D is essential for bone health, oral supplementation has not shown consistent benefits in preventing chronic diseases. This suggests the existence of other mechanisms through which sunlight benefits health. One of the most studied is the photomobilization of nitric oxide (NO) from the skin. UV exposure, especially UVA and UVB, releases NO from cutaneous reservoirs, which dilates arteries
and reduces blood pressure, thus decreasing the risk of cardiovascular diseases.
Mechanisms, nitric oxide, and cardiovascular disease
High blood pressure is the leading cause of disability-adjusted life years worldwide and is responsible for 18% of all global deaths. Population blood pressure correlates directly with latitude, so that about 25% of blood pressure variation can be explained by latitude in the pre-antihypertensive treatment era. Season also has a strong effect on blood pressure.
Measured levels of vitamin D are inversely correlated with blood pressure, so that those with vitamin D levels in the highest quartile have half the odds of having a diagnosis of high blood pressure than those in the lowest quartile. However, oral vitamin D supplements have no effect on blood pressure, so the responsible factor must be an independent effect of vitamin D.
In an epidemiological study of over 340,000 US dialysis patients who have their blood pressure measured three times a week and are treated in over 2,000 different dialysis centers scattered throughout the contiguous United States and followed for over 2 years, we were able to investigate the relationship between UV rays and BP, correcting for temperature and studying the effects of wavelength and skin color on this relationship. We confirmed that, regardless of temperature, UV exposure is inversely correlated with blood pressure and that the beneficial hypotensive effect of UV rays is more pronounced in white Americans than in black Americans and greater for UVB than for UVA.
Myopia and the development of ophthalmologic guidelines on minimum outdoor time
The incidence of myopia is increasing worldwide.
Three generations ago, around 20-30% of children in East Asia had myopia, but now, between 80% and 90% are affected.
Myopia is a risk factor for retinal detachment, glaucoma, and cataracts and is on track to become the leading cause of severe visual impairment and preventable blindness in Europe and worldwide.
Myopia is strongly associated with reduced time spent outdoors, but the association with near work independent of this remains uncertain, and the International Myopia Institute now considers the relationship between reduced outdoor time and myopia to be stronger than the association with near work. Clinical trial data show that increasing the time children spend outdoors reduces the risks of developing myopia and reduces the increase in refractive error.
The mechanism by which spending time outdoors leads to myopia remains uncertain, but the epidemiological and trial data are strong enough for the American Academy of Ophthalmology and the International Myopia Working Group to now recommend that children spend a minimum of 8 to 15 hours per week outdoors to reduce the risk of developing myopia. This contrasts with dermatology advice in the UK for people to avoid sunlight and seek shade between 11 a.m. and 3 p.m.
Other mechanisms and diseases
The concept of the "sunlight quartet" has been proposed to identify diseases that could benefit from UV exposure. This quartet includes conditions that exhibit:
- Latitudinal gradient: Higher prevalence at higher latitudes.
- Seasonal variation: Higher incidence in winter.
- Correlation with vitamin D: Low vitamin D levels associated with higher risk.
- Ineffectiveness of vitamin D supplementation: Supplementation does not reduce risk or severity of the disease.
Examples of diseases meeting these criteria include multiple sclerosis, high blood pressure, type 2 diabetes, and COVID-19. In the case of COVID-19, some studies have shown a correlation between UV exposure and lower mortality, possibly due to virus inactivation by UV radiation and the immunomodulatory effects of sunlight.
Rethinking recommendations
Current evidence suggests a paradigm shift in our view of sunlight is necessary. Recommendations to avoid sunlight exposure need to be reevaluated, taking into account skin color, systemic benefits, and risks to the skin. Further research is needed to fully understand the mechanisms of sunlight action and its long-term health impact.
Key Points
- Sunlight exposure has systemic benefits beyond vitamin D synthesis.
- Photomobilization of skin nitric oxide reduces blood pressure and cardiovascular morbidity.
- Evidence suggests UV exposure could be beneficial for diseases like multiple sclerosis, type 2 diabetes, and COVID-19.
- Recommendations to avoid sunlight need to be reevaluated, considering skin color and systemic benefits.
- Further research into sunlight mechanisms of action and health impact is crucial.
In conclusion, sunlight presents not only risks but also significant health benefits. It’s time to adopt a more balanced approach that allows people to enjoy the benefits of sunlight safely and responsibly, taking into account individual peculiarities and the latest scientific advances.
















