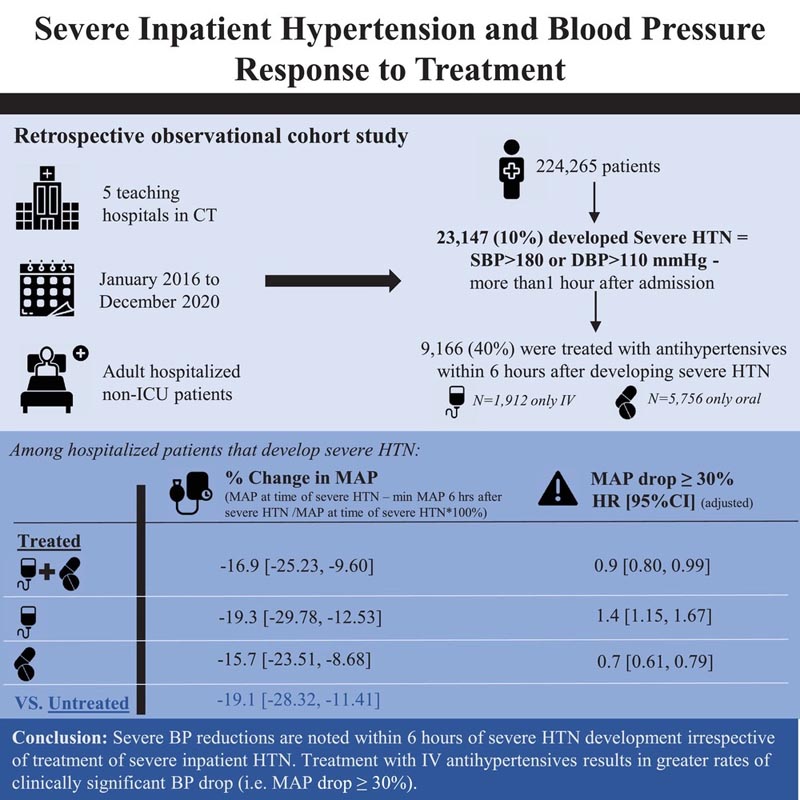
Summary Severe hypertension (HTN) that develops during hospitalization is more common than admission for HT; However, it is poorly studied and treatment guidelines are lacking. Our objective is to characterize hospitalized patients who develop severe HTN and evaluate the blood pressure (BP) response to treatment. This is a multi-hospital retrospective cohort study of adults admitted for reasons other than HTN who developed severe HTN. The authors defined severe in-hospital HTN as the first documented elevation in BP (systolic BP > 180 or diastolic BP > 110) at least 1 hour after admission. Treatment was defined as receiving antihypertensives (intravenous [IV] or oral) within 6 hours of BP elevation. As a measure of possible overtreatment, the authors studied the association between treatment and time to fall in mean arterial pressure (MAP) ≥30% using the Cox proportional hazards model. Among 224,265 hospitalized adults, 10% developed severe HTN, of which 40% were treated. Compared with patients who did not develop severe HTN, those who did develop severe HTN were older, more commonly female and black, and had more comorbidities. The incident MAP drop ≥ 30% between treated and untreated patients with severe HTN was 2.2 vs. 5.7/1000 person-hours. After adjustment, treated versus. untreated patients had lower rates of MAP drop ≥ 30% (hazard ratio [HR], 0.9 [0.8, 0.99]). However, those receiving IV treatment alone versus no treatment had higher rates of MAP decline ≥ 30% (1.4 [1.2, 1.7]). Overall, the authors found that a clinically significant decrease in MAP is observed among hospitalized patients with severe HTN, regardless of treatment , with higher rates observed among patients treated with intravenous antihypertensives alone. More research is needed to determine the phenotype of hospitalized patients with severe hypertension. |
Discussion
In this multi-hospital retrospective cohort study, we found that among adults admitted for reasons other than HTN , severe HTN developed in 10% of whom 40% received antihypertensive treatment, primarily oral medications.
We found that a drop in MAP ≥30% was observed within 6 hours after the development of severe HTN in hospitalized patients, both in treated and untreated patients. After adjusting for demographic and clinical characteristics, untreated patients had higher rates of MAP decline ≥30% compared with treated patients. This association, however, differed depending on the treatment route.
Those treated with oral antihypertensives alone within 6 hours of developing severe HTN had lower rates of MAP fall ≥30% compared with untreated patients. In contrast, those treated with intravenous antihypertensives compared to untreated hospitalized patients had higher rates of MAP fall ≥30%.
The absolute reduction in MAP after the development of severe HTN was slightly greater by 0.6 mm Hg in patients who received treatment (any of the oral antihypertensives) compared to those who did not receive treatment.
We found that treatment with oral antihypertensives could be safer than no treatment, as it resulted in a lower rate of MAP fall ≥30%. This finding persisted even after including only new medication orders. We hypothesized that one possible mechanism by which oral antihypertensives might cause a smaller BP drop compared to no treatment is through attenuation of the rapid BP response. The most common oral antihypertensives administered in this group include metoprolol, amlodipine, and hydralazine.
Conclusions
We found that in a cohort of hospitalized patients admitted for causes other than HTN, 10% of adults developed severe HTN and 40% of these patients were treated with antihypertensives. Paradoxically, treatment (overall and with oral antihypertensives) compared with no treatment resulted in lower rates of MAP decline ≥30%.
Patients with severe HTN treated with IV antihypertensives alone compared with untreated and those treated with oral antihypertensives alone had higher rates of MAP fall ≥30%. Our findings suggest that treatment of severe hospital-acquired HT with intravenous antihypertensives should be performed conservatively .
Upcoming studies will aim to evaluate BP reduction after specific classes and types of antihypertensive drugs and evaluate the effect of treatment on clinical outcomes, such as stroke, myocardial infarction, and AKI, specifically among those with a significant drop in BP. PAM.
Since both treated and untreated patients with severe HTN had a significant reduction in MAP, a one-size-fits-all approach is not appropriate for treating severe HTN.
Furthermore, it is essential to conduct prospective studies using standardized BP measurement to evaluate the frequency of severe HTN, as well as the role of treatment on outcomes. Finally, more research is needed to phenotype hospitalized patients with severe HTN based on risk of adverse outcomes to help establish personalized treatment guidelines.
Comments
In the absence of guidelines, it remains arbitrary to treat patients who develop substantially elevated blood pressure (BP) during hospitalization. The researchers conducted a retrospective cohort study of more than 200,000 hospitalized adult patients who were not critically ill (with diagnoses other than hypertensive emergency) at five teaching hospitals in Connecticut. Approximately 23,000 patients met criteria for severe hypertension (defined as systolic BP >180 mm Hg or diastolic BP >110 mm Hg), and 9,000 of them received treatment: 21% received intravenous (IV) medications, 63% received oral medications, and 16% received both.
The primary outcome was a drop in mean arterial pressure of >30%, a measure of potential harm . In the adjusted analysis of treated versus untreated patients , those who received only intravenous antihypertensive treatment were significantly more likely to have this potentially adverse outcome (hazard ratio, 1.4), and those who received only oral antihypertensive medications were significantly more likely to have this potentially adverse outcome (hazard ratio, 1.4), and those who received only oral antihypertensive medications were significantly lower (HR, 0.7).
A takeaway from the current study, consistent with others, is that the use of intravenous antihypertensives should be discouraged in hospitalized noncardiac patients without end-organ damage.
Elevated blood pressure in hospitalized patients is often related to factors such as fluctuating pain and agitation and spontaneous falls without treatment. The apparent benefit of oral antihypertensive agents observed in this study could be due to residual confounding and is antithetical to another recent large study, in which treatment of hospitalized patients who developed hypertension was associated with an excess risk of acute kidney injury and myocardial infarction, with no benefit observed even at severe BP ranges
















