Diabetic retinopathy (DR) remains the leading cause of blindness in working-age adults and the fifth most common cause of preventable blindness. Prevention of DR relies on effective control of hyperglycemia with the goal of achieving near-normal blood glucose as soon as possible after diagnosis and continuing to achieve the target HbA1c range over time.
Data from clinical trials suggest that β-cell decline occurs more rapidly and that failure to achieve glycemic goals with oral agents is more common and occurs earlier in patients diagnosed with youth-onset type 2 diabetes compared with those with onset of type 2 diabetes later in life. The challenge of effectively managing youth with type 2 diabetes is compounded by the social and economic burdens of these youth, who largely represent underserved racial and ethnic minorities.
Therefore, physiological and socioeconomic barriers combine to place youth with type 2 diabetes at very high risk for rapidly worsening glycemic control and potentially more rapid progression of diabetes-related complications, including DR.
In the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study and its follow-up observational study, TODAY2, participants were monitored with longitudinal assessments of diabetes control and DR progression from 2004 to 2020.
Two rounds of standard stereoscopic testing of seven field digital background photography were conducted in 2010-2011 and ~7 years later in 2017-2018. Although with only a short mean duration of diabetes at the time of the first fundus photograph (mean 4.9 years, range 2 to 8), TODAY study participants had a DR prevalence of 13.9 %. The TODAY/TODAY2 study investigators recently published the longitudinal prevalence of complications over a median follow-up period of 10 years, reporting that the prevalence of all complications had increased and the prevalence of DR increased to 49%.
With the marked increase in the prevalence of DR and the presence of sight-threatening lesions, understanding the modifiable risk factors that drive the progression of DR during the transition from youth to young adulthood with type 2 diabetes is essential to preserve the long-term vision, which is essential for future physical functioning, financial employment opportunities and overall quality of life. We now report risk factors associated with DR progression in youth-onset type 2 diabetes.
Aim
The Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study reported a 13.9% prevalence of diabetic retinopathy (DR) in youth with a mean ± SD duration of type 2 diabetes of 4.9 ± 1. 5 years. After 7 years of additional follow-up, we report risk factors for DR progression in the TODAY cohort.
Methodology
Retinal photographs (n = 517) were obtained in 2010-2011 and again in 2017-2018 (n = 420) with standard seven-field stereoscopic digital fundus photography. Photographs were graded centrally using the Early Treatment Diabetic Retinopathy Study (ETDRS) scale.
A total of 367 patients with gradeable fundus photographs in at least one eye at both evaluations were included in the analyzes of DR progression, defined as an increase of three or more steps on the ETDRS scale.
Results
With a mean ± SD age of 25.4 ± 2.5 years and diabetes duration of 12.0 ± 1.5 years, there was a 49% prevalence of any DR among participants.
The prevalence by stage of DR was as follows: 39% for very mild or mild nonproliferative DR (NPRD), 6% for moderate to severe NPRD, and 3.8% for proliferative DR. Compared with those who did not progress, participants who advanced three or more steps had significantly lower BMI, higher HbA1c, higher blood pressure, increased triglycerides, decreased C-peptide, and a higher prevalence of other comorbidities.
Multivariate analysis demonstrated that HbA1c was the dominant factor affecting DR progression.
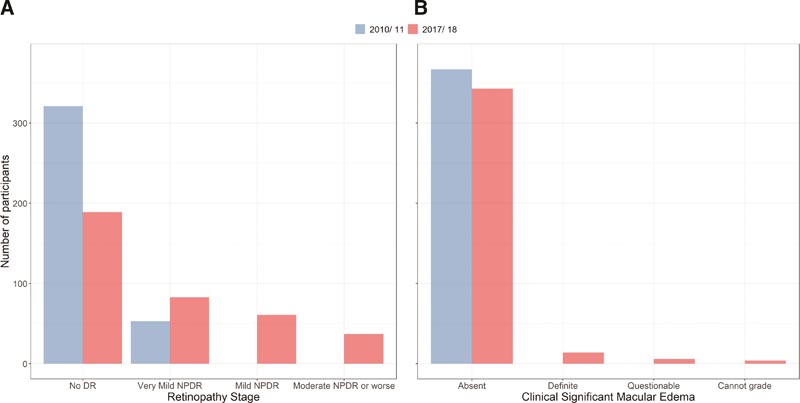
Cohort results (N = 367) with standard seven-field fundus examinations during TODAY (2010–2011) and TODAY2 (2017–2018) for DR (A) and CSME (B).
Conclusions Poor glycemic control in youth-onset type 2 diabetes carries a high risk for progression of DR, including advanced sight-threatening disease in young adulthood. |
Discussion
After ~10 years of follow-up and an average diabetes duration of 12 years, almost half of the TODAY study participants developed DR. In the 7 years between retinal evaluations, participants progressed from very mild NPDR at baseline evaluation to more advanced stages of DR, including 5% of participants who progressed to severe NPDR or PDR despite having, on average, only 25 years old. CSME, not detected at baseline evaluation, was present in 3.8% of participants at fundus photography 7 years later.
Prevalence rates of DR in younger patients with type 2 diabetes have been reported from other cross-sectional studies in various populations and have ranged from 4 to 37% (16–19). Notably, these studies included wide age ranges for diabetes diagnosis, spanned longer durations of diabetes, and involved varied methods for detecting DR. Our results rigorously confirm the presence and progression of advanced retinal pathology over only 7 to 8 years in youth-onset type 2 diabetes.
Of clinical concern, the prevalence of DR in our cohort is almost double the 28.5% prevalence reported for adults with type 2 diabetes older than 40 years with an average diabetes duration of 15 years, as previously reported by the National Health and Nutrition Examination Survey (NHANES).
Perhaps the elevated prevalence and accelerated progression of DR in youth-onset type 2 diabetes or T2D compared with adult-onset type 2 diabetes reflects the challenge of achieving and maintaining euglycemia in youth. The high rates of early treatment failure (i.e., defined as HbA1c ≥8% for 6 months or sustained metabolic decompensation requiring insulin) observed in the TODAY trial suggested that youth were less responsive to the oral therapies used and experienced more loss. Rapid endogenous insulin production by β cells compared to adults.
In fact, even with an average diabetes duration of only about a decade, those who experienced a progression of 3 steps or more in DR classification had many of the well-recognized risk factors for DR from studies of adults with diabetes: Higher HbA1c, blood pressure, and triglycerides as well as the presence of diabetic kidney disease.
Not surprisingly, as in adults with short-duration type 2 diabetes, multivariate analyzes identified glycemic control as the predominant risk factor for the development and progression of DR. However, unlike studies of adult-onset type 2 diabetes, men in our cohort were no more likely than women to experience DR progression.
As this cohort ages, it could be hypothesized that hypertension and hyperlipidemia will play larger roles, heralding concern about the proposed association of early retinal vascular changes with later cardiovascular disease risk. Future studies could include more detailed retinal vascular imaging to investigate the retina-heart connection in patients with youth-onset type 2 diabetes.
This is the first comprehensive report on risk factors for DR progression in youth-onset type 2 diabetes. Strengths of the study include the longitudinal study design and the systematic analysis of fundus photographs taken by masked raters using the ETDRS scale in the TODAY/TODAY2 study. Although not all TODAY participants completed both retinal assessments, the participants studied are a representative cohort, with no significant differences in clinical characteristics at TODAY baseline between those with repeat fundus examinations and the full TODAY cohort.
Although baseline retinal evaluation was performed early in the course of youth-onset type 2 diabetes, it is not a true baseline retinal evaluation at the time of diabetes diagnosis. However, because only a minority of participants (13.9%) had developed retinopathy no more severe than very mild NPDR at the time of initial evaluation, this is a compelling baseline for developmental analysis. and disease progression.
Given the accelerated decline in β-cell function documented among patients with youth-onset type 2 diabetes and the predominant role of glycemia in the progression of DR, the detection and identification of at-risk youth with obesity who belong to historically underserved populations for type 2 diabetes should occur routinely in clinical care and research should continue to identify additional treatment options.
For youth with type 2 diabetes, aggressive glycemic control from the time of diagnosis accompanied by recommended annual screening for the development and progression of DR, with additional more intensive monitoring as warranted by diabetes status. disease, is essential to preserve vision in adulthood.
















