Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age, with a prevalence of 5% to 18%. PCOS used to be considered primarily a reproductive condition ; However, it is now commonly accepted that women with PCOS are at high risk for metabolic disorders , such as obesity, glucose intolerance, type 2 diabetes mellitus (T2DM), metabolic syndrome, and possibly cardiovascular events. Additionally, women with PCOS have been shown to have an increased risk of psychological morbidity, 10, 11 asthma, 12 and migraine. 13
Surprisingly, only a few studies have systematically evaluated overall comorbidity in women with PCOS. This should be a high priority given the high cost to society that results from PCOS-related morbidity. For example, PCOS-related T2DM alone has been estimated to carry an annual cost of £237 million ($310 million) in the UK15 and $1.77 billion in the US.
It often remains underdiagnosed and therefore underrepresented in patient and national registries, limiting the capture of comorbidities. Previous studies mainly reported hospital diagnoses without data on symptoms. Furthermore, attention has focused primarily on women in their early or middle reproductive years, and morbidity data in late childbearing age are scarce.
The present study focused on evaluating morbidities, self-reported symptoms, medication use, and health care service use in 46-year-old women with PCOS and in controls without PCOS who were part of the Northern Birth Cohort. Finland based on population (NFBC).
Material and methods
The study population came from the 1966 Northern Finland Birth Cohort and consisted of women who reported oligo/amenorrhea and hirsutism at the age of 31 years and/or a diagnosis of PCOS at the age of 46 years (n = 246 ) and controls without symptoms or diagnosis of PCOS (n = 1573), referred to as women without PCOS.
The main outcome measures were self-reported data on symptoms, diagnosed illnesses, and use of medications and healthcare services at age 46 years.
Results
The risk of overall morbidity increased by 35% (risk ratio [RR] 1.35, 95% confidence interval [CI] 1.16–1.57) and medication use by 27% [RR 1 .27, 95% CI 1.08–1.50] compared with women without PCOS, and the risk remained after adjusting for body mass index.
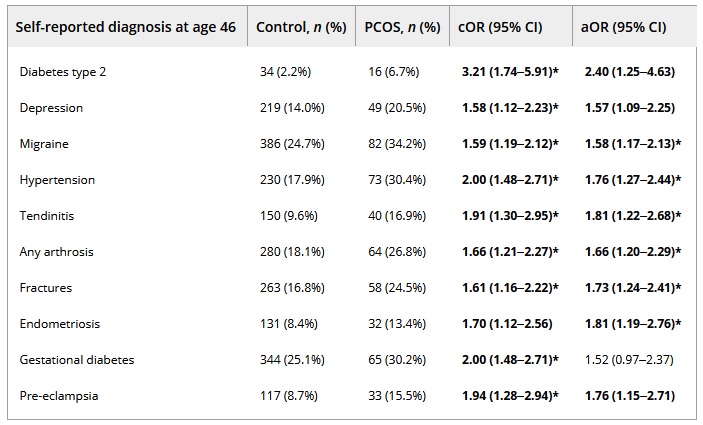
The diagnoses with the highest prevalence in women with PCOS were migraine, hypertension, tendinitis, osteoarthritis, fractures and endometriosis .
PCOS was also associated with autoimmune diseases and recurrent upper respiratory tract infections and symptoms. Interestingly, the use of health care services did not differ between the study groups after adjusting for body mass index.
Table: Self-reported diagnosis at age 46
Conclusions
Women with PCOS are burdened with multimorbidity and increased medication use, regardless of body mass index.
Discussion
This population-based follow-up study illustrates the high risk of multimorbidity and poor self-rated health among women with PCOS through their late reproductive years. We show that PCOS is associated with an increased risk of several diseases and symptoms, some of them related, for the first time, to PCOS.
Some of the differences in disease risk, and especially in medication use, were due to high BMI, indicating that PCOS, per se, may not always be the root cause of some of the comorbidities. However, the median morbidity score of PCOS women with a BMI of 25 kg/m2 or more was similar to that of PCOS women with lower weight. Further studies on the pathogenetic mechanisms of comorbidities in PCOS are warranted, as high BMI appears not to be solely responsible for increased morbidity.
At age 46, women with PCOS had a higher risk of T2DM, depression, migraine, hypertension, tendinitis, osteoarthritis (especially of the knee, back, or shoulder), fractures, endometriosis, gestational diabetes, and preeclampsia , although after adjustments , the risks of T2DM, depression, gestational diabetes, and preeclampsia were no longer significantly increased.
In fact, it has been established that normal weight women with PCOS are not at risk of developing T2DM, especially in Nordic populations. Metabolic conditions , such as hypertension and T2DM, are well established in PCOS and are also related to the risk for preeclampsia. A previous study specifically evaluated cardiovascular disease in this population, showing that the risk of hypertension increases in PCOS, independent of obesity, and that the risk of CVD events increases up to age 49 years.
We have also reported adverse metabolic reactions for women with PCOS, as well as recorded cardiac morbidity. Controversially, an increased risk of long-term CVD has not been detected in studies with older populations.
Our study also revealed an increased risk of migraine in PCOS, in line with existing literature. Further studies on the mechanism are warranted, as migraine is often related to hormonal fluctuations of the menstrual cycle that are often altered in PCOS.
It remains to be determined whether the higher prevalence of endometriosis is related to more extensive gynecologic evaluations in this subfertile population or to long-acting estrogen and progesterone resistance in PCOS.
Tendonitis has not been linked to PCOS before ; However, general musculoskeletal diseases and osteoarthritis are more common in affected women. The risk of fracture among women with PCOS is debatable. In a Danish population, fractures were not more common, in contrast to a Taiwanese study as well as ours.
We have recently reported higher levels of vitamin D in the same PCOS population; however, markers of bone formation and bone mineral density appear to be decreased in PCOS. More studies should be conducted among PCOS women with different phenotypes to segregate the role of hyperandrogenism and metabolic disorders.
Respiratory tract problems were more common in women with PCOS. Women reported having cough with wheeze, recurrent respiratory infections, and atopic, infantile, or allergic eczema more frequently than controls. Evidence of a higher prevalence of various respiratory infections and diseases in women with PCOS is increasing.
The mechanisms behind these disorders are unknown, but increased low-grade systemic inflammation or hyperandrogenism may be predisposing factors.
The increased prevalence of eczema is a novel finding, although some dermatological manifestations, such as hidradenitis suppurativa, have previously been linked to PCOS.
This is the first study to evaluate self-reported symptoms related to infections and autoimmune diseases among women with PCOS. Affected women more frequently reported recurrent infections, including pneumonia, otitis, and common colds, and a greater susceptibility to infections than controls at age 46 years.
Additionally, symptoms related to autoimmune diseases were more common in women with PCOS than in controls. These results are supported by a recent systematic review and meta-analysis that present women with PCOS not only at increased risk of autoimmune thyroid disease but also at increased risk of asthma .
There is only one previous population-based study on medication use among women with PCOS. Although the increase in medication use in our study was self-reported, the medication profile was similar to that reported in the Danish registry-based study. Medications used to treat the alimentary tract and metabolic diseases were more common in polycystic ovary syndrome.
This group of medications includes not only metformin , but also medications for gastric problems. The finding of increased use of medications for functional gastrointestinal disorders may reflect higher levels of stress and anxiety, which have been shown to cause gastrointestinal symptoms, as well as an increased risk of irritable bowel syndrome in PCOS.
The use of medications targeting the cardiovascular system was higher in PCOS, as we reported in our previous publication. Beta blocker use was higher in women with PCOS than in controls. Since the first-line treatment for high blood pressure is medications targeting the renin-angiotensin system, beta-blocking agents may have been prescribed for indications other than hypertension, such as anxiety symptoms, which are highly prevalent in the PCOS, as is sympathetic arousal.
The increased use of medications that affect the nervous system in PCOS was expected, given the psychological morbidity related to the syndrome.
Additionally, increased use of medications to treat skin manifestations in PCOS was observed, likely explained by acne, hirsutism, and male-type hair loss commonly associated with the syndrome. Since our study also showed a higher prevalence of atopic eczema and other autoimmune symptoms in PCOS, more research should be conducted targeting the dermatological manifestations related to the syndrome.
Women with PCOS reported morbidities, symptoms, and increased medication use more frequently than controls. Furthermore, women with PCOS rated their health as poor or very poor almost three times more often compared to controls, in line with our previous finding. In line with this, affected women reported more frequent healthcare visits, although this seemed driven by high BMI.
Our study emphasizes multimorbidity and poor self-perceived health among women with PCOS.
Further studies are warranted to explore the disease mechanisms in more detail.
Final message Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age. In a study published in Acta Obstetricia et Gynecologica Scandinavica, women with PCOS were more likely than other women to be diagnosed with migraine, hypertension, tendonitis, osteoarthritis, and endometriosis . Affected women also used medications more frequently and reported their own health to be poorer than women without PCOS. The study included 246 women with symptoms or diagnoses of PCOS and 1,573 controls who were surveyed during their final reproductive years at age 46. “PCOS is often labeled as a reproductive problem; However, in most cases this is managed well with fertility treatments. “Our study underscores the need for healthcare professionals to recognize the risk of several comorbidities and increased health burden related to this common syndrome,” said senior author Professor Terhi T. Piltonen, MD, PhD, of the University from Oulu, in Finland. “Women should also be aware of this risk and should be supported by early diagnosis and treatment.” |
















