Summary
Piriformis syndrome is a subgroup of deep gluteal syndrome , an important differential diagnosis of sciatica. The piriformis is a short external rotator muscle of the hip joint that passes close to the sciatic nerve as it passes through the large sciatic foramen.
Compression causes numbness, pain, or tingling in the buttocks, posterolateral aspect of the leg, and foot . The causes of sciatic nerve entrapment in deep gluteal syndrome are best shown by endoscopic examination. However, the frequency of anatomical variants in normal subjects should warn that such anomalies are not necessarily the cause of the symptoms.
Most people have experienced temporary leg numbness after sitting uncomfortably or for too long on a toilet seat or hard chair. This is perhaps a benign variant of deep gluteal syndrome. It is caused by compression or irritation of the sciatic nerve located within or adjacent to the greater sciatic notch.
Piriformis syndrome is a subgroup of deep gluteal syndrome, first described by Yeoman in 1928 as sciatica caused by arthritis of the sacroiliac joint, piriformis muscle, and adjacent branches of the sciatic nerve. Other causes of entrapment within the subgluteal space are fibrous and vascular bands (inferior gluteal artery), obturator internus/gemini syndrome, and ischiofemoral pathology.
Before endoscopic exploration, the validity of this diagnostic label was uncertain since there were no defined criteria or specific tests at the time, although many had been proposed. In an article of 18 studies and 6,062 cadavers, the prevalence of piriformis and sciatic nerve anomalies in cadavers was 16.9%; almost identical to the 16.2% in ’surgical cases’.
Anatomy
The piriformis muscle is a short external rotator muscle of the hip joint that stretches with internal rotation of the leg. H. Crooke described it in 1615 as:
“The fourth extensor called Iliacus externus piriformis, the pear muscle of the hip outwards... because it fills the external and inferior cavity of the hip bone with its oblique position, and is like a round pear.”
Figure 1. Piriformis and sciatic nerve.
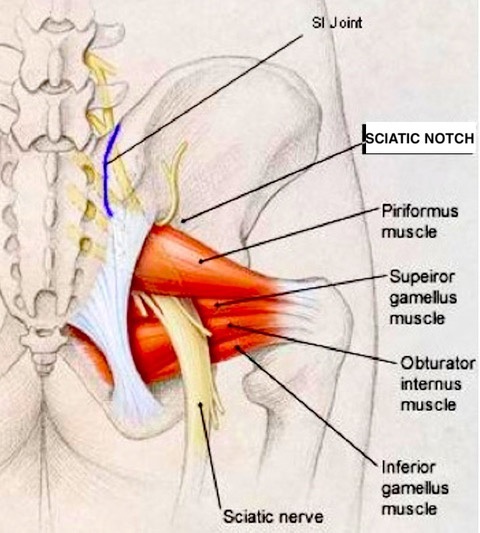
Its origin is from the anterior surface of the sacrum; It inserts into the greater trochanter through a tendon that fuses with the tendons of the obturator internus and the gastrocnemius muscles. The sciatic nerve exits the pelvis through the large sciatic foramen, usually below the piriformis. (Figure 1) There are several anatomical variations in the relationship between the piriformis muscle and the sciatic nerve, which can lead to nerve irritation or entrapment. The undivided nerve may pass below or through the piriformis or may divide above the piriformis into the lateral tibial and popliteal nerves with one portion exiting through the piriformis and the other below.
Clinical features
As a differential diagnosis from sciatica caused by much more common disc injuries, piriformis syndrome is characterized by numbness or pain in the buttocks that occurs after prolonged sitting, cycling, or excessive or repeated exercise. Back pain is not a feature. In most cases, mild numbness, pain, or tingling in the buttocks, posterolateral aspect of the leg, and foot disappears after a few minutes of standing or walking.
In less frequent but more serious cases , the symptoms are persistent. Typical but non -diagnostic physical signs are:
|
Research
In an MRI study of 783 cases, there were no significant differences in the prevalence of piriformis syndrome, buttock pain, or sciatica between normal and variant sciatic nerve anatomy. Piriformis syndrome is probably overdiagnosed . Only if symptoms are persistent or disabling should investigations be used to exclude discogenic lumbosacral root compression, sacroiliac joint dysfunction, and spinal, paraspinal and pelvic masses.
In such cases, investigations are useful, but none are diagnostic . The causes of sciatic nerve entrapment in the deep gluteal region are best shown by endoscopic examination .
The main use of MRI is to exclude lumbosacral spinal etiologies. MRI may be normal or show hypertrophy/atrophy, fibrosis, or abnormal insertion of the piriformis. MR neurography may show asymmetry of the piriformis muscle and hyperintensity of the sciatic nerve in the sciatic notch.
Increased latency of the H reflex in nerve conduction studies and electromyographic denervation in muscles innervated by the sciatic nerve are variably but unreliably recorded .
The study by Han et al, after excluding other spinal or pelvic pathology, proposed diagnostic criteria . (Table 1) The frequency of anatomical variants in normal subjects, however, should caution that such anomalies are not necessarily the cause of the symptoms.
Table 1. Proposed diagnostic characteristics
Piriformis syndrome is diagnosed if 4 or more criteria are met. |
Treatment
Most cases are benign and self-limiting if provoking factors are avoided. A bewildering variety of treatments have been used, many with imperfectly controlled studies, most with high success rates. They include: anti-inflammatory medications, physical therapy, piriformis stretching, injection of local anesthetics or corticosteroids, and botulinum toxin injections.
Periarticular endoscopic decompression of the sciatic nerve is less invasive than exploratory surgery and, in intractable cases, is useful in elucidating the various causes of deep gluteal syndrome and providing means to correct the causative lesions. Thirty-nine of 52 patients had good to excellent results in a recent review.
Muscle resection with or without neurolysis of the sciatic nerve should be a last resort , but was considered "satisfactory in 10 of 12 patients who did not respond to more conservative treatments."















