The COVID-19 pandemic and its impacts have taken a disproportionate toll on American mothers who were pregnant or had recently given birth. Maternal mortality (i.e., deaths during pregnancy or in the early postpartum period) increased by 18% in 2020, according to data from the National Center for Health Statistics, outpacing the ~16% increase in overall US mortality. in 2020. However, according to a new analysis from the University of Maryland and Boston University, the maternal mortality rate after the start of the COVID-19 pandemic was even higher and disproportionately affected Hispanic mothers. black and not white.
A research letter published in JAMA Network Open by Marie Thoma at the UMD School of Public Health and Eugene Declercq at the BU School of Public Health compared maternal mortality data from 2018 to March 2020, when the pandemic began, with April to December 2020. Overall, they found large increases in maternal deaths (33%) and late maternal deaths (41%) after March 2020 compared to before the pandemic, and notable increases among Black and Hispanic mothers .
“The increase was really driven by deaths after the start of the pandemic, which are higher than what we see in overall excess mortality in 2020,” said Dr. Thoma, assistant professor of family sciences at UMD. SPH. The study also showed that existing and new disparities emerged after the pandemic with a 40% increase among already high rates for non-Hispanic Black women and a 74% increase among previously lower rates for Hispanic women.
Surprisingly, said Dr. Declercq, a professor of community health sciences at BUSPH, “for the first time in more than a decade, the maternal mortality rate for Hispanic women during the pandemic was higher than that of non-white women.” Hispanics, a change that may be related to COVID and deserves greater attention in the future.”
COVID-19 was included as a secondary cause of death in 14.9% of maternal deaths in the last nine months of 2020, being a contributing factor for 32% of Hispanic women, 12.9% of African American women, and 7% of non-Hispanic white women.
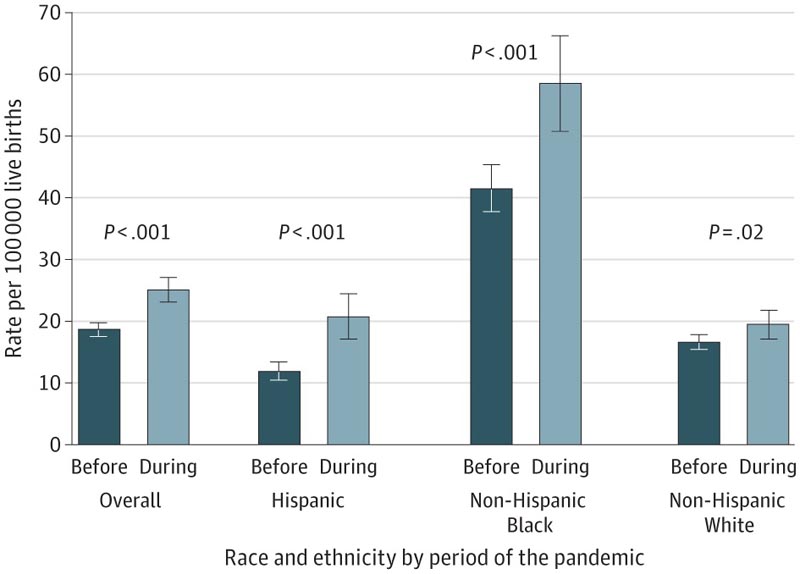
Analysis of maternal mortality after the start of the COVID-19 pandemic showed a 40% increase among already high rates for non-Hispanic Black women and a 74% increase among previously lower rates for Hispanic women.
In their analysis of the causes of maternal death, they found that the largest increases were due to conditions directly related to COVID-19 (respiratory or viral infection) and conditions that worsened with COVID-19 infection, such as diabetes or cardiovascular diseases . However, disruptions to the health care system could have led to a delay in prenatal care that could have meant that risk factors for pregnancy complications went undetected.
“We need more detailed data on the specific causes of maternal deaths in general and those associated with COVID-19,” Dr. Thoma said. “We could possibly see improvements in 2021 due to vaccine rollout, as well as the extension of postpartum care provided to Medicaid recipients as part of the American Rescue Act of 2021 in some states. “We will continue to examine this.”
Conclusions In the US, maternal deaths increased substantially (33.3%) after March 2020, corresponding to the onset of COVID-19, higher than the 22% of the estimated overall excess deaths associated with pandemic. The increases were highest for Hispanics and non-Hispanic blacks. women. The change in maternal deaths during the pandemic may involve conditions directly related to COVID-19 (respiratory or viral infection) or conditions exacerbated by COVID-19 or other interruptions in health care (diabetes or cardiovascular diseases)5, but could not be discerned from the data. Limitations of the study include the large percentage of COVID-19 cases with a non-specific underlying cause (reflecting a maternal death coding issue6) and data partitioning that resulted in small numbers for some categories (rates were suppressed). for <16 deaths). Future studies of maternal death should examine the pandemic’s contribution to racial and ethnic disparities and should identify specific causes of maternal deaths in general and associated with COVID-19. |
















