Highlights
• Ketogenic diet therapy resulted in reversal of metabolic syndrome in this severe mental illness cohort.
• Participants with schizophrenia showed an average improvement of 32% on the Brief Psychiatric Rating Scale.
• The percentage of participants with bipolar disorder who showed >1 point improvement in clinical global impression was 69%.
• Greater biomarker benefits were observed with adherence to the ketogenic diet.
• A pilot trial suggests dual metabolic and psychiatric benefits of ketogenic therapy.
Summary
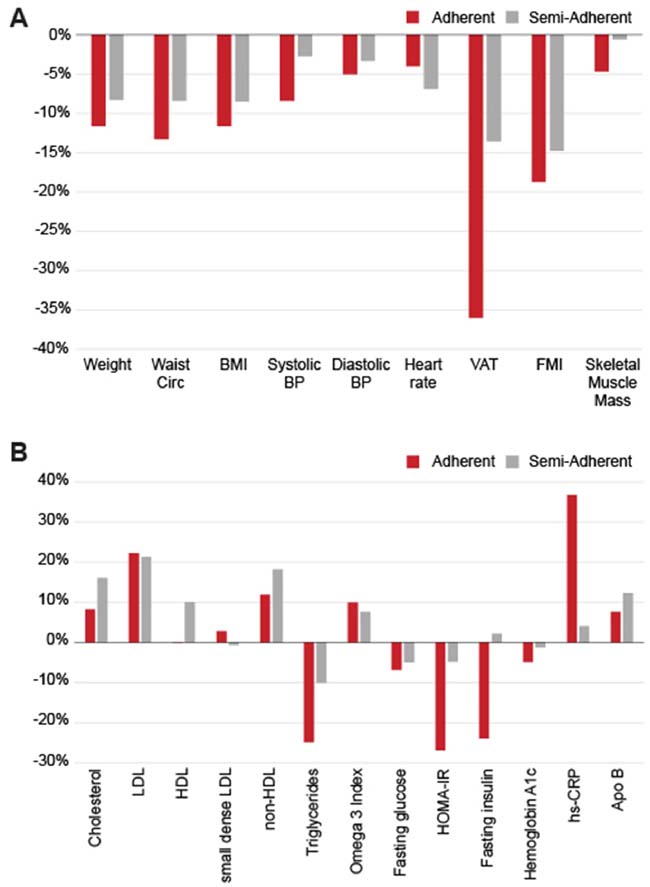
The ketogenic diet (KD, also known as metabolic therapy ) has been successful in treating obesity, type 2 diabetes, and epilepsy. More recently, this treatment has shown promise in the treatment of psychiatric illnesses. We conducted a 4-month pilot study to investigate the effects of a ketogenic diet (KD) in people with schizophrenia or bipolar disorder with existing metabolic abnormalities. Twenty-three participants were enrolled in a single-arm trial. The results showed improvements in metabolic health, and no participants met the criteria for metabolic syndrome at the conclusion of the study. Adherent individuals experienced a significant reduction in weight (12%), BMI (12%), waist circumference (13%), and visceral adipose tissue (36%). Biomarker improvements seen in this population include a 27% decrease in HOMA-IR and a 25% drop in triglyceride levels.
On psychiatric measures, participants with schizophrenia showed a 32% reduction in Brief Psychiatric Rating Scale scores. Overall Clinical Global Impression (CGI) severity improved by an average of 31%, and the proportion of participants starting with elevated symptomatology improved by at least 1 CGI point (79%). Psychiatric outcomes across the entire cohort encompassed increased life satisfaction (17%) and improved sleep quality (19%). This pilot trial highlights the potential benefits of complementary ketogenic dietary treatment in people suffering from serious mental illness.
Standard treatment with antipsychotic medications presents a complex challenge for individuals with severe mental illnesses like schizophrenia or bipolar disorder. While these medications effectively manage brain chemistry, they often come with significant metabolic side effects such as insulin resistance and obesity, which can be distressing enough to lead some patients to discontinue treatment.
In a recent pilot study led by researchers from Stanford Medicine, a ketogenic diet has emerged as a potential solution to not only restore metabolic health in these patients alongside their ongoing medication regimen but also to enhance their psychiatric conditions. Published in Psychiatry Research on March 27, the findings suggest that dietary intervention could play a pivotal role in mental illness treatment.
Dr. Shebani Sethi, associate professor of psychiatry and behavioral sciences and lead author of the study, expressed optimism about the results: "It´s very promising and encouraging that we can potentially regain some control over the disease, in addition to standard care."
Dr. Sethi, who holds certifications in obesity and psychiatry, first noticed the potential of the ketogenic diet during her time as a medical student in an obesity clinic. She encountered a patient with treatment-resistant schizophrenia whose auditory hallucinations improved significantly on the diet, prompting her to explore existing medical literature. While historical case reports linked ketogenic diets with schizophrenia treatment, their effectiveness in epilepsy treatment provided a compelling basis for further investigation.
"The ketogenic diet works by reducing neuronal excitability in the brain, which has proven effective in treatment-resistant epilepsy," explained Dr. Sethi. This insight led her to pioneer the concept of "metabolic psychiatry," a novel approach to mental health focusing on energy metabolism.
During the four-month pilot study, Dr. Sethi´s team monitored 21 adult participants diagnosed with schizophrenia or bipolar disorder. These individuals were already on antipsychotic medications and had metabolic issues such as weight gain or insulin resistance. They were instructed to follow a ketogenic diet comprising approximately 10% carbohydrates, 30% protein, and 60% fat, with an emphasis on whole foods like proteins and non-starchy vegetables.
"The diet emphasizes unprocessed whole foods and does not restrict fats," Dr. Sethi noted, highlighting that participants received practical guidance and resources such as keto cookbooks and access to a health coach.
Weekly measurements of blood ketone levels tracked participants´ adherence to the diet throughout the study period. By the end of the trial, 14 patients were fully compliant with the diet, six were partially adherent, and only one was non-adherent.
The study underscores the potential of ketogenic dietary therapy as a complementary approach to managing severe mental illnesses, offering hope for improved outcomes in metabolic and psychiatric health.
Participants in the study underwent a series of psychiatric and metabolic assessments throughout the trial.
Prior to starting the trial, 29% of participants met the criteria for metabolic syndrome, which includes conditions such as abdominal obesity, high triglycerides, low HDL cholesterol, high blood pressure, and elevated fasting glucose levels. After following the ketogenic diet for four months, none of the participants met the criteria for metabolic syndrome anymore.
On average, participants experienced a 10% reduction in body weight, an 11% decrease in waist circumference, and improvements in blood pressure, BMI, triglyceride levels, blood sugar, and insulin resistance.
"We´re observing significant changes," noted Sethi. "Even while taking antipsychotic medications, we were able to reverse obesity, metabolic syndrome, and insulin resistance. This is very encouraging news for patients."
The study also revealed unexpected psychiatric benefits. Participants, on average, showed a 31% improvement on the Clinical Global Impressions Scale, a tool used to assess the severity of mental illness by psychiatrists. Three-quarters of the participants demonstrated clinically meaningful improvement. Additionally, participants reported enhancements in sleep quality and overall life satisfaction.
"Participants noted improvements in their energy levels, sleep patterns, mood, and overall quality of life," said Sethi. "They feel healthier and more optimistic."
Researchers were particularly impressed by the high adherence rate to the ketogenic diet among participants. "We observed greater benefits in those who adhered strictly to the diet compared to those who were partially adherent, suggesting a potential dose-response relationship," Sethi remarked.
Alternative Fuel for the Brain
There is mounting evidence suggesting that psychiatric disorders such as schizophrenia and bipolar disorder may arise from metabolic deficiencies in the brain, affecting the excitability of neurons, according to Sethi.
Researchers speculate that just as a ketogenic diet enhances overall bodily metabolism, it may also improve brain metabolism.
"Improving overall metabolic health is likely to benefit brain health as well," Sethi explained. "However, the ketogenic diet uniquely offers ketones as an alternative energy source for a brain experiencing energy dysfunction."
Sethi added that there are likely multiple mechanisms at play, and the primary objective of the small pilot study is to identify signals that will inform the design of larger, more robust studies.
In her clinical practice, Sethi encounters many patients dealing with serious mental illnesses along with obesity or metabolic syndrome, yet few studies have focused on this underserved population. She is the founder and director of Stanford Medicine´s metabolic psychiatry clinic.
"Many of my patients struggle with both conditions, so my goal was to explore if metabolic interventions could provide relief," she stated. "They are seeking solutions to feel better."
The study, involving researchers from the University of Michigan, the University of California, San Francisco, and Duke University, was supported by the Baszucki Group Research Fund, the Keun Lau Fund, and the Foundation for the Treatment of Obesity.
















