Sarcopenia, a progressive skeletal muscle disorder characterized by loss of muscle mass and strength, represents a major global health burden, especially among older adults. It was officially recognized as a disease in 2016.
It affects up to 10% of people over the age of 60 and has profound implications for healthcare systems worldwide. Its social effects are significant: directly, it contributes to increased healthcare costs (recurrent hospitalizations, need for long-term care); indirectly, it reduces independence and quality of life (QoL), as physical performance declines, the risk of falls and fractures increases, and difficulties arise in performing basic and instrumental activities of daily living (ADL and IADL).
Sarcopenia has been identified as a public health priority requiring immediate attention.
Preventive interventions usually focus on a combination of nutritional, exercise, and, more recently, pharmacological strategies. However, despite its importance, identification and treatment remain an ongoing challenge due to long-standing differences and debates stemming from the lack of universally accepted operational definitions.
The prevalence of sarcopenia varies widely depending on the definition used. Furthermore, the effectiveness of approaches aimed at improving patient-centered outcomes such as QoL remains limited.
In this context, the Global Leadership Initiative in Sarcopenia (GLIS) was established. This initiative seeks to standardize the definition and diagnostic criteria for sarcopenia into a unified classification that could serve as the gold standard.
GLIS aims to standardize the definition and diagnostic criteria of sarcopenia in a unified, common framework. This includes definitions of sarcopenia that best predict health outcomes, preferred tools for measuring these outcomes, and the cut-off points defining normal and abnormal values.
Methodology
GLIS has established the following working groups (WG):
- Muscle strength
- Muscle mass
- Sarcopenia outcomes
First, the three leaders of the WG on sarcopenia outcomes conducted a literature review to identify key outcomes. GLIS members drafted, reviewed, and approved a list of seven outcomes.
Seven subgroups were then created to investigate:
(i) Influence of sarcopenia on physical performance and mobility
(ii) Influence of sarcopenia on instrumental and basic activities of daily living (functional independence)
(iii) Influence of sarcopenia on quality of life
(iv) Relationship between sarcopenia and fall-related fractures
(v) Prevalence and implications of sarcopenia in hospitalized populations
(vi) Role of sarcopenia in predicting admission to nursing homes
(vii) Association between sarcopenia and mortality
With a high level of evidence, sarcopenia is significantly associated with lower QoL, higher risk of falls and fractures, and higher mortality risk. Findings suggested that muscle strength and physical performance were more closely related to QoL than muscle mass alone.
The largest differences in QoL were observed when using the AWGS (Asian Working Group for Sarcopenia) criteria.
Evidence was found of a direct association between sarcopenia and various outcome measures. A heatmap representation showed levels of evidence for several outcomes, categorized as high (++), moderate (+), or low (-); NA = not applicable, ADL = activities of daily living, IADL = instrumental activities of daily living.
Systematic reviews, meta-analyses, and observational studies reviewed by the GLIS Outcome WG and its seven subgroups revealed that sarcopenia is consistently associated with several key clinical outcomes.
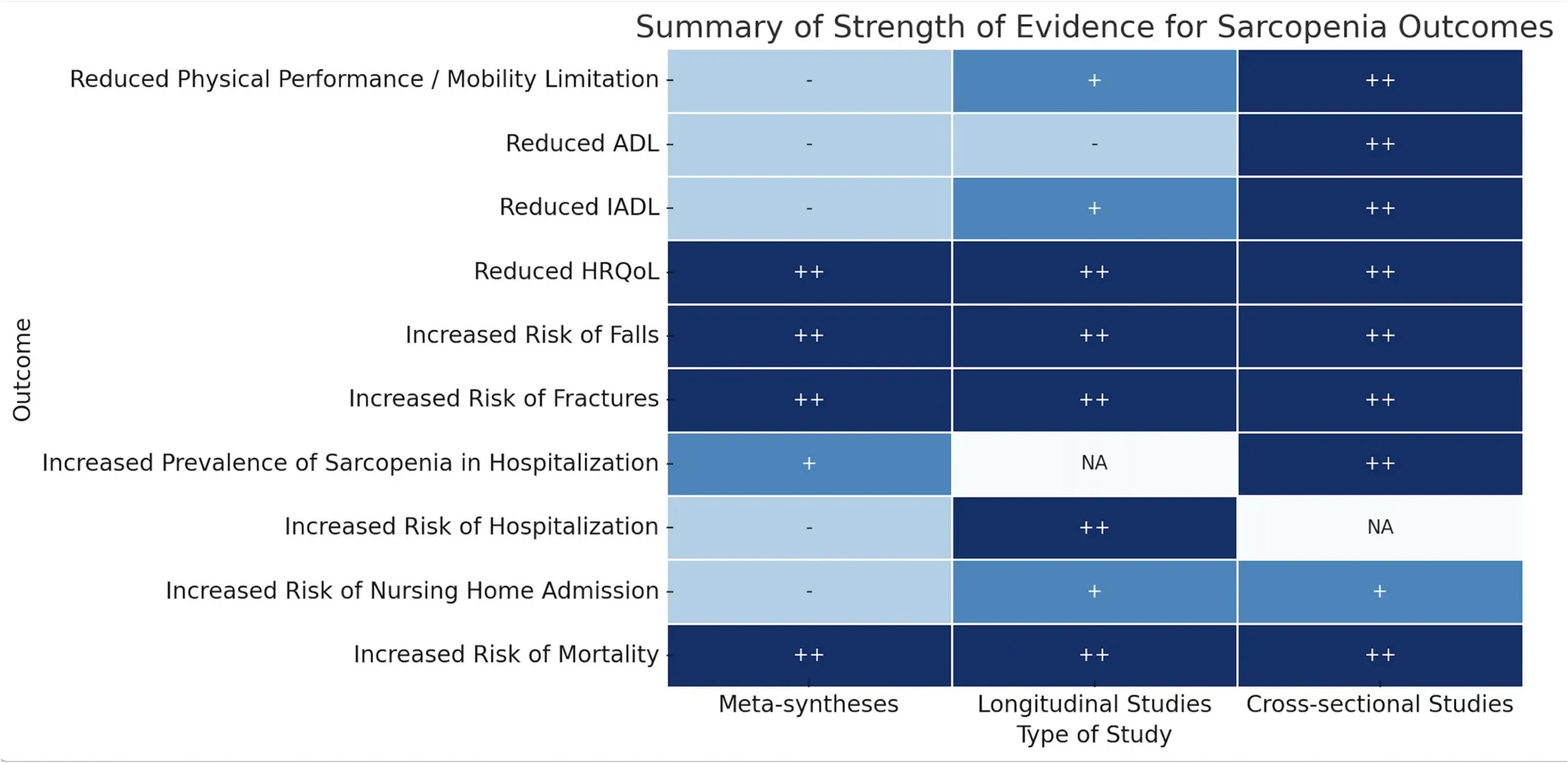
The following associations were identified with a high level of evidence from metasyntheses and longitudinal and cross-sectional studies:
• Higher mortality risk: Numerous metasyntheses have shown that sarcopenia nearly doubles the risk of mortality, regardless of diagnostic criteria. When considering sarcopenia components separately, reduced muscle strength appears to be the strongest predictor of death, while reduced muscle mass alone shows less consistent findings.
• Reduced health-related QoL: The negative influence of sarcopenia on health-related QoL has been widely reported, particularly among nursing home residents and when using sarcopenia-specific assessment tools. A large meta-analysis including 43 cross-sectional studies revealed that individuals with sarcopenia had significantly lower QoL scores than those without the condition. The smallest differences were seen using the EWGSOP1 (European Working Group on Sarcopenia in Older People) criteria, and the largest using AWGS criteria. When analyzing sarcopenia components separately, another systematic review found that muscle strength and physical performance—rather than muscle mass alone—were more closely associated with health-related QoL.
• Higher risk of falls and fractures: Numerous metasyntheses have reported this association regardless of diagnostic criteria. A higher risk of falls was mainly observed in community-dwelling individuals rather than nursing home residents, suggesting context-specific differences. When analyzing components separately, evidence suggests that muscle strength is more strongly associated with fracture risk, while muscle mass correlates with low bone mass.
A reduction in IADL associated with sarcopenia has been found in both cross-sectional and longitudinal observational studies, though an exception has been noted among nursing home residents. Most available data come from populations with sarcopenia diagnosed using EWGSOP1 criteria.
When analyzing components separately, one meta-analysis highlighted that reductions in muscle mass, strength, and physical performance predict declines in IADL over time. However, evidence linking sarcopenia with reduced ADL remains inconclusive. One longitudinal and two cross-sectional studies found no association, while three other cross-sectional studies did report a significant association between sarcopenia and reduced ADL.
Regarding hospitalization risk, while studies agree that sarcopenia prevalence is high among hospitalized older adults, whether sarcopenia predicts hospitalization is less clear. Roughly half of the studies found no significant association, while the other half reported a significantly higher risk of hospitalization among individuals with sarcopenia.
Evidence linking sarcopenia with nursing home admissions is also scarce. Only a low level of evidence was found in metasyntheses and a moderate level in longitudinal and cross-sectional studies.
Evidence from multiple studies clearly indicates that sarcopenia has a significant negative impact on quality of life. This relationship is most evident when using sarcopenia-specific assessment tools such as the SarQoL (Sarcopenia Quality of Life) questionnaire and the AWGS diagnostic criteria.
















