Background
The benefits of endoscopic removal of small (≤6 mm) asymptomatic kidney stones are unknown. Current guidelines leave such decisions to the urologist and the patient. A prospective study involving older non-endoscopic technology and some retrospective studies favor observation.
However, published data indicate that approximately half of the small kidney stones remaining at the time the larger stones were removed caused other symptomatic events within 5 years of surgery.
Methods
We conducted a multicenter, randomized, controlled trial in which, during endoscopic removal of ureteral or contralateral kidney stones, small remaining asymptomatic stones were removed in 38 patients (treatment group) and were not removed in 35 patients (control group). The primary outcome was relapse measured by future emergency department visits, surgeries, or secondary stone growth.
Results
After a mean follow-up of 4.2 years , the treatment group had a longer time to relapse than the control group (P<0.001 by log-rank test). The restricted mean time (±SE) to relapse was 75% longer in the treatment group than in the control group (1631.6±72.8 days vs. 934.2±121.8 days).
The risk of relapse was 82% lower in the treatment group than in the control group (hazard ratio, 0.18; 95% confidence interval, 0.07 to 0.44), at 16%. of patients in the treatment group who had a relapse compared to 63% of those in the control group. Treatment added a median of 25.6 minutes (interquartile range, 18.5 to 35.2) to surgery time.
Five patients in the treatment group and four in the control group visited the emergency department within 2 weeks of surgery. Eight patients in the treatment group and 10 in the control group reported passing kidney stones.
Conclusions
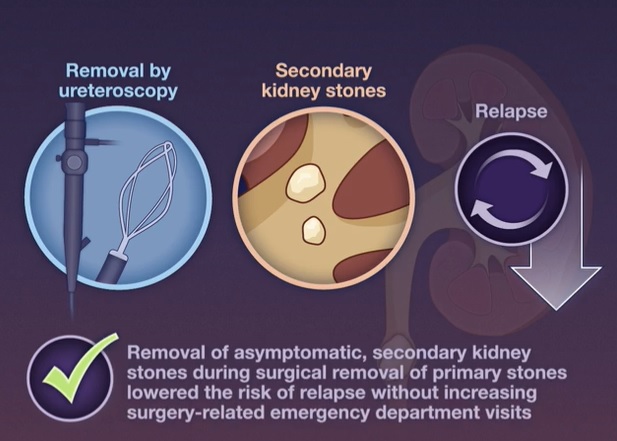
Removal of small, asymptomatic kidney stones during surgery to remove ureteral or contralateral kidney stones resulted in a lower incidence of relapse than nonremoval and a similar number of surgery-related emergency department visits.
(Funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the Puget Sound Veterans Affairs Health Care System; ClinicalTrials.gov number, NCT02210650)
Comments
Elimination of asymptomatic kidney stones, a randomized trial
Removal of small asymptomatic stones during a procedure to remove a symptomatic stone prevented subsequent symptomatic stone events.
Some patients who undergo ureteroscopic removal of symptomatic ureteral or kidney stones also have small, asymptomatic kidney stones. Because some of those asymptomatic stones will eventually cause symptoms, should they be routinely removed when treating the symptomatic stone?
The investigators enrolled 73 patients who were scheduled for removal of a symptomatic primary kidney or ureteral stone, and who also had one or more additional asymptomatic kidney stones (size ≤6 mm). Patients were randomized to ureteroscopic removal of the symptomatic stone and asymptomatic ipsilateral or contralateral stones (the treatment group) or to ureteroscopic removal of only the primary symptomatic stone (the control group).
During the median follow-up of 4 years, patients in the treatment group were significantly less likely than controls to have stone-related emergency department visits or additional stone-related surgeries (11% vs. 43%).
Although surgery time was longer in the intervention group (by an average of 25 minutes), the authors report no difference in complication rates between the groups.
In this study, prophylactic removal of small asymptomatic kidney stones (during ureteroscopy to remove a symptomatic one) prevented subsequent stone events, apparently without excessive adverse effects.
In an informal conversation with a urologist, I learned that current US practice varies, often depending on the patient’s overall clinical condition, the patient’s prior experience with symptomatic stones, and the personal preferences of the patient and urologist. This study could help promote informed decision making.















