A cross-sectional study found that human papillomavirus (HPV) was more likely to be diagnosed in women born in the 1980s compared to women born in the 1990s.
The human papillomavirus (HPV) vaccine was recommended for routine use beginning in 2006 for young women aged 9 to 26 years. To evaluate the vaccine’s effectiveness, a study published in JAMA Health Forum compared the likelihood that women born in the 1980s and 1990s would be diagnosed with HPV. The researchers found that women born in the 1990s had a lower risk of HPV.
In the US, human papillomavirus (HPV) vaccination was first recommended for routine use among girls and young women (ages 9 to 26) in 2006.1 Steady improvements in vaccination coverage against HPV over the last decade may have translated into protective benefits among the contemporary birth cohort (i.e., women born in the 1990s compared to the 1980s).
To measure whether HPV vaccination has been associated with reduced infection rates between vaccinated newborn women (vaccine-mediated immunity) and unvaccinated women (herd protection), we compared HPV prevalence in the birth cohorts of the 80s and 90s and a pre-vaccination period versus a recent period. period.
Methods
The institutional review board at the University of Texas Health Science Center deemed this study exempt from review and waived the informed consent requirement because only publicly available data were used. We follow the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
This cross-sectional study analyzed data from 2 waves (2005-2006 and 2015-2016) of the National Health and Nutrition Examination Survey (NHANES), a stratified multistage probability sample of the civilian population in the US. Demographic characteristics, including immunization history and race and ethnicity, were self-reported and collected by trained interviewers during an in-home interview.
Participants provided self-collected cervicovaginal swab samples that were evaluated by polymerase chain reaction testing and then type-specific hybridization was performed.
We estimated the prevalence of infection of HPV types 16 and 18 (HPV-16/18), the oncogenic types covered by the quadrivalent vaccine, for 2 birth cohorts: women born in the 1980s (1980-1989) and the 1990s (1990-1998). ).
To estimate the effectiveness of HPV vaccination, we estimated the prevalence of HPV-16/18 infection before vaccine introduction (2005-2006) and recently (2015-2016) from NHANES data.
Considering that the 1990s birth cohort was 26 years old or younger in 2015 and 2016, we limited the comparison to the 18–26 year old age groups. Additionally, we performed multivariable logistic regression to assess differences in estimated probabilities, with simultaneous adjustments made for number of vaccine doses, age, race and ethnicity, country of birth, age at sexual debut, and age. number of sexual partners throughout life.
Data analyzes were performed from November 2021 to February 2022 with SAS, version 9.4 (SAS Institute Inc) using SAS PROC SURVEY procedures, 3 which included weight, cluster, strata, and domain statements. Statistical significance was tested at 2-tailed P < 0.05.
Results
The study sample comprised 2,698 women aged 18 to 26 years (mean [SD] age, 21.5 [2.7] years; 879 [32.6%] white). The prevalence of HPV-16/18 among participants born in the 1990s was statistically significantly lower (5.6%; 95% CI, 4.0%-7.2%) than those born in the 1980s (12.5%; 95% CI, 10.2%-14.7%). %; Figure, A).
During the 2015-2016 cycle, 55% of women ages 18 to 20, 52% of women ages 21 to 23, and 50% of women ages 24 to 26 had received 1 or more doses of the vaccine. HPV. Among women aged 18 to 26 years, the prevalence of HPV-16/18 before the introduction of vaccination (2005-2006 cycle) was 15.2% (95% CI, 11.2%-19.1 %). In the recent period (2015-2016), this percentage had decreased to 3.3% (95% CI, 1.3%-5.3%) overall: 5.1% (95% CI, 1.2% -9.1%) among the unvaccinated and 1.0% (95% CI, 0.0%-2.5%) among the vaccinated groups (Figure, B and C). The prevalence of HPV-16/18 infection in the recent period (2015-2016) was 0% among unvaccinated and vaccinated women aged 18 to 20 years.
The estimated probability of HPV-16/18 infection was 54% lower for women born in the 1990s (6.3%; 95% CI, 5.7%-6.9%) than in the 1990s. 1980 (13.6%; 95% CI, 12.7%-14.4%.
Similarly, the estimated probability was 78% lower overall during the 2015-2016 cycle (3.5%; 95% CI, 2.9%-4.1%) compared to the 2005-2006 cycle ( 15.7%; 95% CI, 14.0%-17.4%). ); more specifically, 60% lower for the unvaccinated (6.3%; 95% CI, 5.0%-7.4%) and 92% lower for the vaccinated (1.2%; 95% CI, 1 .0%-1.3%).
Estimated probabilities were lower for the 1990s (vs. 1980s) birth cohort and for the recent period (2015-2016) vs. pre-vaccination (2005-2006) across race and ethnicity categories. , number of sexual partners throughout life and country of birth.
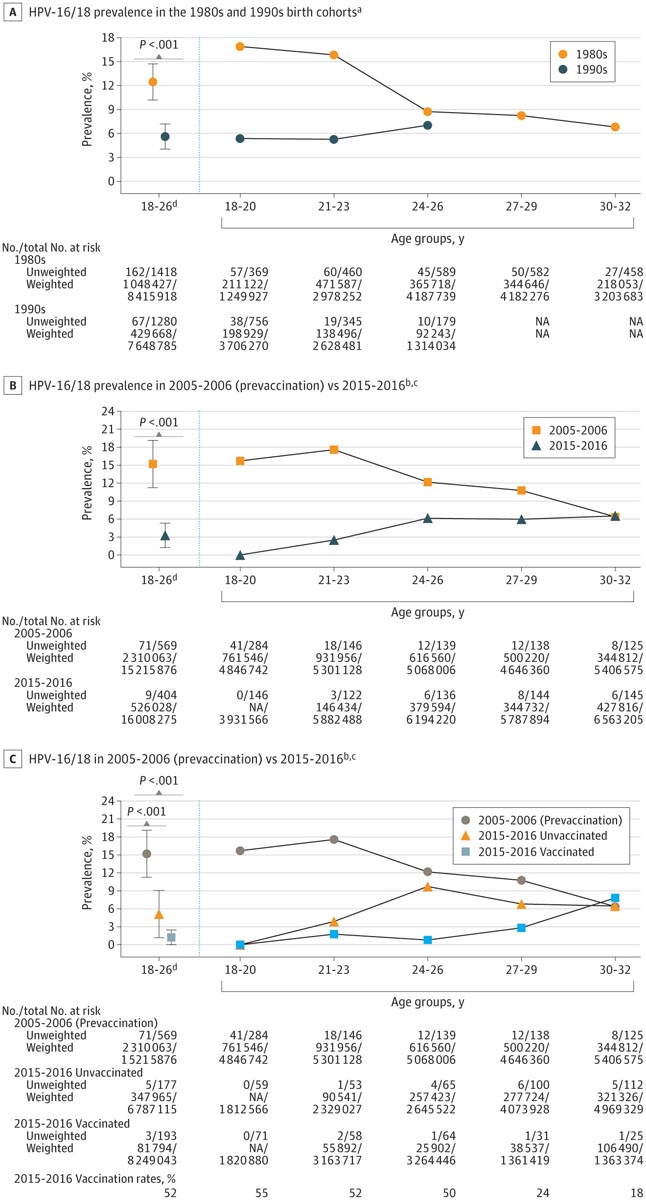
Prevalence estimates of HPV-16/18 infection among women born in the 1980s and 1990s and during the pre-vaccination period (2005-2006) versus the recent vaccination period (2015-2016), overall and by HPV vaccination status
Discussion
The findings of this study suggest that HPV vaccination was associated with a reduction in the prevalence of HPV-16/18 infection among a newborn cohort of vaccinated and unvaccinated women aged 18 to 26 years. A further decline in the prevalence of HPV-16/18 infection among women aged 18 to 20 years during 2015-2016 may reflect greater direct and collective protection from broader HPV vaccination coverage.
These findings are consistent with a recent study demonstrating the effectiveness of HPV vaccination. Additionally, this study provides a birth cohort perspective and suggests a shift in the age distribution of HPV-16/18 prevalence. Limitations of the study were the use of self-reported HPV vaccination status and the exclusion of HPV types not covered by the vaccine.
Historically in the US, the prevalence of HPV infection among women has followed a log-normal distribution pattern, with the peak observed among young age groups. This fundamental concept may need to be reevaluated for HPV-16/18 infection, given the recent peak shift we observed.
The researchers concluded that HPV infection in women was lower in those born in the 1990s and in the post-vaccination period (2015-2016) across all demographics compared to those born in the 1980s and women from the cycle prior to vaccination (2005-2006).
















