Guidelines on pulmonary hypertension call for earlier diagnosis
The European Society of Cardiology (ESC) and European Respiratory Society (ERS) Guidelines for Diagnosis and Treatment recommend earlier detection of pulmonary hypertension in the community and expeditious referral of complex or high-risk patients. of pulmonary hypertension, published in European Heart Journal and European Respiratory Journal.
“The diagnosis of pulmonary hypertension, and therefore the initiation of appropriate treatment, is often considerably delayed,” said the chair of the ESC guidelines working group, Professor Stephan Rosenkranz of the University Hospital of Cologne, Germany. “In young patients, often women, delays are often due to disbelief of a serious illness in an otherwise healthy-looking young individual. In older patients, symptoms may be attributed to coexisting diseases (such as hypertension, obesity, or cardiopulmonary diseases) and pulmonary hypertension is missed. “Patients with shortness of breath should seek medical help and if the GP, cardiologist or pulmonologist cannot identify an appropriate reason, referral to an expert pulmonary hypertension center is indicated.”
Pulmonary hypertension affects approximately 1% of the world’s population and up to 10% of people over 65 years of age. It refers to high blood pressure in the pulmonary circulation and differs from "hypertension," which is high blood pressure in the arteries that supply the rest of the body. People with this condition have thick, stiff pulmonary arteries that cause the right side of the heart to constantly work harder to push blood, ultimately leading to right heart failure. Pulmonary hypertension is a serious condition associated with a substantially reduced life expectancy if not successfully treated. Recent studies have shown that even moderately elevated pulmonary artery pressure or pulmonary vascular resistance is associated with increased mortality. This is why the hemodynamic definitions had to be updated.
There are no specific symptoms, but patients typically suffer from progressive shortness of breath with exertion and a reduced ability to exercise. Climbing stairs can be difficult. Many patients experience chronic fatigue and fluid retention may occur as a result of impaired right heart function. Other symptoms include chest pain, dizziness, and fainting, particularly in those with advanced right heart failure.
Chair of the ERS guidelines working group, Professor Marion Delcroix from University Hospitals Leuven, Belgium, said: "Being diagnosed with pulmonary hypertension, often after considerable delay, and feeling physically limited has a tremendous psychological impact. , emotional and social in patients and their families". “Psychosocial support is recommended in patients with pulmonary arterial hypertension (PAH), who often develop depression and anxiety and have to reduce work.”
Pulmonary hypertension is divided into five main groups depending on the cause: 1) PAH, which is a distinct pulmonary vascular disease; 2) pulmonary hypertension associated with left heart disease; 3) pulmonary hypertension associated with chronic lung disease; 4) chronic thromboembolic pulmonary hypertension (CTEPH) due to recurrent blood clots in the lungs; and 5) pulmonary hypertension of unclear and/or multifactorial causes.
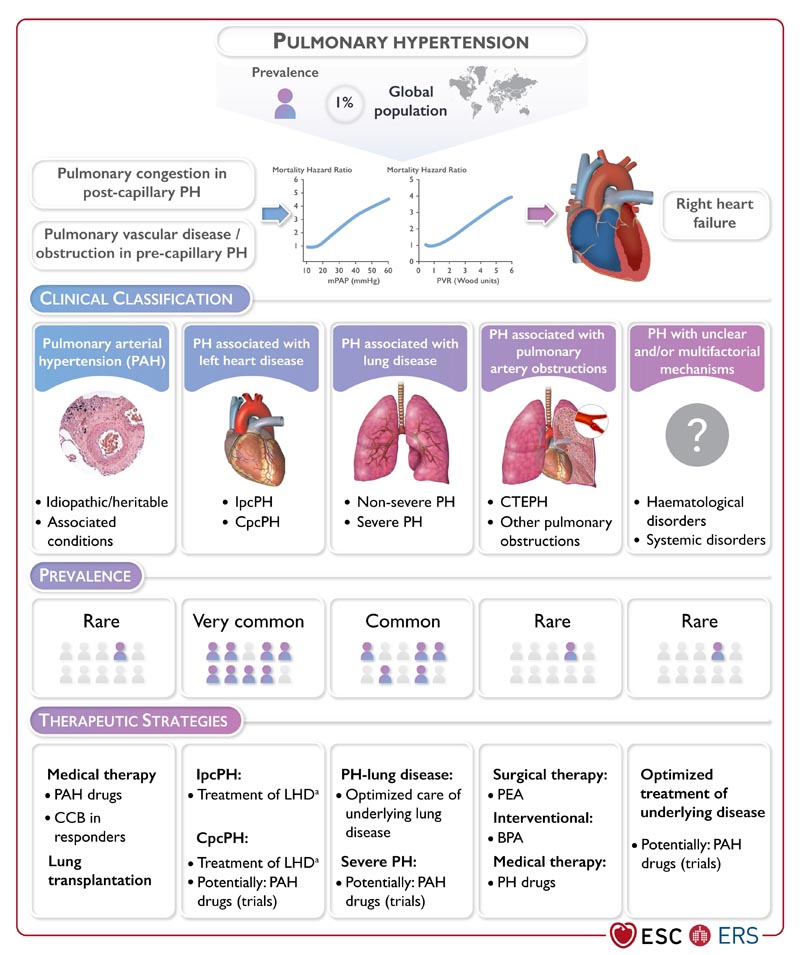
The guidelines cover the entire spectrum of pulmonary hypertension with emphasis on the diagnosis and treatment of PAH and CTEPH. For PAH, early diagnosis and initiation of treatment are key. Treatment options have improved over the past 15 years and three classes of medications are currently approved. Most patients should receive a combination of at least two medications. Treatment decisions should be guided by the risk assessment strategy described in the document. Immunization of patients with PAH against COVID-19, influenza, and pneumococcal disease is recommended.
In women with PAH, pregnancy may be associated with a substantial risk of maternal complications or even maternal death, especially when PAH is not well controlled with medical treatment. Therefore, it is recommended that women of childbearing potential with PAH be counseled at the time of diagnosis about the risks and uncertainties associated with pregnancy; This should include advice on not getting pregnant and referrals for psychological support when necessary.
There are three options for the treatment of CTEPH, which can be used alone or in combination. Pulmonary endarterectomy is the surgical removal of thromboembolic lesions of the pulmonary arteries and is the preferred strategy in eligible patients. Balloon pulmonary angioplasty is indicated in some patients who are not suitable for surgery or who have persistent or recurrent pulmonary hypertension after surgery. During this procedure, a balloon is temporarily inserted into the pulmonary arteries via a catheter, which is then inflated to move thromboembolic lesions and restore blood flow. The third treatment option is medication . Individual treatment strategies should be discussed in high-volume centers with multidisciplinary teams.
Multidisciplinary input is central to the management of pulmonary hypertension. This is because a number of conditions can cause pulmonary hypertension, with left heart disease and chronic lung disease being the most common underlying causes. Additionally, other conditions such as connective tissue disease, liver disease, human immunodeficiency virus (HIV) infection, and congenital heart disease can cause PAH. Finally, a variety of imaging techniques, including computed tomography, cardiovascular magnetic resonance imaging, and echocardiography, are required to detect lung disease and chronic or recurrent pulmonary embolism, and to monitor the structure and function of the right heart.
















