Nearly half of pregnancy-related deaths occur during hospitalizations, more than a quarter of which may occur after delivery, and the pregnancy-related mortality rate is increasing in the hospital setting. 1 , 2 This study aimed to examine long-term trends in inpatient mortality rates among pregnant and postpartum individuals and the proportion of deaths by period of pregnancy (prenatal, delivery, and postpartum).
Methods
The Centers for Disease Control and Prevention determined that this cross-sectional study was exempt from institutional review board review and informed consent because it was a secondary data analysis of de-identified data. This study followed the STROBE reporting guideline. Using data from the National Inpatient Sample from 1994 to 2015 and 2017 to 2019, 3 we examined patterns of inpatient mortality during pregnancy-associated hospitalizations.
Inpatient mortality was identified based on discharge disposition, which was missing in less than 0.01% of observations. From 1994 to 2015, we assessed temporal trends in the inpatient mortality rate by pregnancy period and their statistical significance using recursively calculated orthogonal polynomial coefficients for linear trend tests.
Results
Between 1994 and 2015, an estimated 12,654 inpatient deaths occurred among pregnant and postpartum women with a mean age (standard error [SE]) of 29.37 (0.14) years among 84,181,338 hospitalizations (mean age [SE ], 27.47 [0.001] years).
Regression analyzes revealed that inpatient deaths during intrapartum hospitalizations decreased from 10.6 (95% CI, 8.3 to 12.9) deaths per 100,000 intrapartum hospitalizations (788 inpatient deaths hospitalizations among 7,423,264 hospitalizations during childbirth) to 4.7 (95% CI, 3.5 to 5.8) deaths per 100,000 hospitalizations for childbirth (310 inpatient deaths among 6,661,065 hospitalizations for childbirth) among 1994 to 1995 and 2014 to 2015 (absolute change = –5.9 [95% CI, –8.5 to –3.4] deaths per 100,000 birth hospitalizations; P < .001).
The rate of inpatient deaths in the prenatal and postpartum periods remained unchanged between 1994 and 1995 and between 2014 and 2015 (Figure 1). From 1994 to 2015, the overall in-hospital mortality rates for prenatal and postpartum hospitalizations were 4.5 (95% CI, 4.1 to 4.9) and 3.0 (95% CI, 2.7 to 3. 3) deaths per 100,000 hospital deliveries, respectively.
An estimated 1,480 inpatient deaths (mean [SE] age, 31.31 [0.44] years) and 10,898,224 birth hospitalizations (mean [SE] age, 28.89 [<0.001] years) were identified. between 2017 and 2019; the rates of death from prenatal, delivery, and postpartum hospitalizations were, respectively, 2.9 (95% CI, 2.2 to 3.7), 6.1 (95% CI, 5.1 to 7.2), and 4.5 (95% CI, 3.6 to 5.4) deaths per 100,000 hospital deliveries. In 2017 to 2019, prenatal and postpartum hospitalizations accounted for 6.2% and 2.3% of perinatal hospitalizations, but 21.6% and 33.1% of inpatient deaths occurred during these periods, respectively.
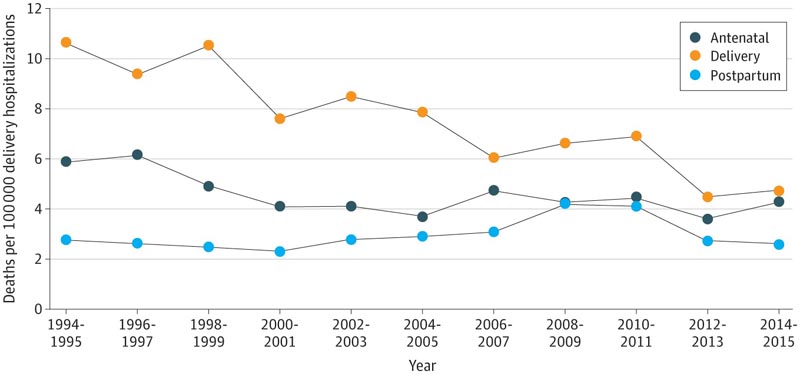
Figure: Trends in hospital mortality among pregnancy hospitalizations. Data are from the national sample of hospitalized patients. Temporal trends in the hospital mortality rate associated with each pregnancy period were assessed using recursively calculated orthogonal polynomial coefficients. The p value was calculated for these linear trend tests. All analyzes were performed using SAS statistical software version 9.4 (SAS Institute), with two-sided tests and a threshold α = 0.05.
Discussion
This cross-sectional study found that between 1994 and 1995 and 2014 and 2015, the inpatient death rate during intrapartum hospitalizations decreased by 56% , while the inpatient death rates during prenatal and postpartum hospitalizations did not. they changed During 2017 to 2019, prenatal and postpartum hospitalizations accounted for less than 10% of hospitalizations but more than half of hospital deaths among pregnant and postpartum people.
Resources devoted to improving the quality of care in obstetric delivery have been associated with lower rates of severe morbidity and may be associated with lower mortality identified during hospitalizations during childbirth. However, clinical and policy efforts may need to be additionally directed toward prenatal and postpartum hospitalizations and structural factors associated with increased risk of adverse prenatal and postpartum outcomes.
Limitations of this study include modeling assumptions and reliance on cross-sectional administrative data, which may be subject to coding errors and misclassification. Future research is needed to identify and address inequities in in-hospital maternal morbidity and mortality stratified by individual, community, and structural factors.
Comments
One study suggests that maternal deaths in hospitals occur earlier in pregnancy or postpartum, while maternal deaths that occur at the time of delivery are declining in the US.
Hospitalizations that occur in the prenatal period, or during pregnancy but before childbirth, and those that occur in the postpartum period, accounted for more than half of in-hospital maternal deaths between 2017 and 2019, a new study reveals.
The findings, published in JAMA Network Open , estimated rates of in-hospital maternal deaths from the National Inpatient Sample for the years 1994 to 2015 and 2017 to 2019 among prenatal, delivery, and postpartum hospitalizations in the United States.
"Maternal mortality rates are high in the United States, higher than those seen in all other industrialized countries," said lead author Lindsay Admon, MD, MSc, assistant professor of obstetrics and gynecology at the US School of Medicine. University of Michigan and obstetrician and gynecologist at the University of Michigan Von Voigtlander Women’s Hospital.
“Maternal mortality continues to rise in the U.S., and we wanted to understand trends in hospital deaths: Are they occurring during pregnancy, childbirth, or postpartum? Has this changed over time? Ultimately, we wanted to generate data that could help design clinical and policy interventions to prevent the most adverse of all obstetric outcomes in the hospital setting, maternal death.
In their recent study, Admon and his co-authors found that during the 20-year period between 1994-1995 and 2014-2015, in-hospital maternal deaths that occurred at the time of delivery fell by more than half (56%). During the same period, rates of in-hospital maternal deaths that occurred during the prenatal and postpartum periods remained unchanged.
Looking at the most recent data from 2017 to 2019, the research team found that birth hospitalizations accounted for nearly 90% of hospitalizations that occurred during pregnancy up to a few weeks after delivery, but only half of maternal deaths. at the hospital.
In contrast, prenatal and postpartum hospitalizations accounted for less than 10% of all hospitalizations that occurred during pregnancy up to a few weeks after delivery, but half of the in-hospital maternal deaths identified.
“It is important to note that there appears to be progress in reducing the rate of maternal death at the time of childbirth,” Admon said. “At the same time, we know that maternal mortality continues to rise in the U.S. To further reduce rates of maternal deaths that occur in the hospital, we must focus not only on the time of delivery, but also on examining the risks and the complications that occur during childbirth and the postpartum as well.”
Perinatal quality collaboratives and resources, such as patient safety bundles provided by The Alliance for Innovation on Maternal Health, have been implemented in US hospitals to reduce preventable maternal mortality, and research has shown that In many cases, this has improved maternal morbidity and mortality rates at the time of delivery.
With this new study, Admon says there needs to be a renewed focus on examining the causes of maternal death in the hospital during periods of pregnancy other than childbirth.
“We are ready to delve deeper into this work and determine the main drivers of maternal deaths that occur during prenatal and postpartum hospitalizations and whether they differ from those that influence birth-related outcomes,” he explained.
“Detailed reviews of each case are very important. “Once root causes are identified, clinical and policy changes can be more clearly directed toward improving maternal health and reducing maternal morbidity and mortality.”
Reference : “ Trends and Distribution of In-Hospital Mortality Among Pregnant and Postpartum Individuals by Pregnancy Period ” DOI: 10.1001/jamanetworkopen.2022.24614
















