Summary
Goals :
The “ 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease” provides recommendations to guide clinicians in diagnosis, genetic evaluation and familial screening, medical therapy, endovascular and surgical treatment, and surveillance. long-term monitoring of patients with aortic disease worldwide and their multiple clinical presentation subsets (i.e., acute, stable symptomatic, and asymptomatic aortic syndromes).
Methods:
A comprehensive literature search was conducted from January 2021 to April 2021, covering studies, reviews and other evidence conducted on human subjects that were published in English in PubMed, EMBASE, the Cochrane Library, CINHL Complete and other relevant selected databases. for this guide. . The writing committee also considered additional relevant studies, published through June 2022 during the guideline writing process, where appropriate.
Structure:
Previously published AHA/ACC guideline recommendations on thoracic aortic disease, peripheral arterial disease, and bicuspid aortic valve disease have been updated with new evidence to guide clinicians. Additionally, new recommendations have been developed that address the comprehensive care of patients with aortic disease. There is additional emphasis on the role of shared decision making , especially in the management of patients with aortic disease both before and during pregnancy. There is also greater emphasis on the importance of institutional intervention volume and multidisciplinary aortic team expertise in the care of patients with aortic disease.
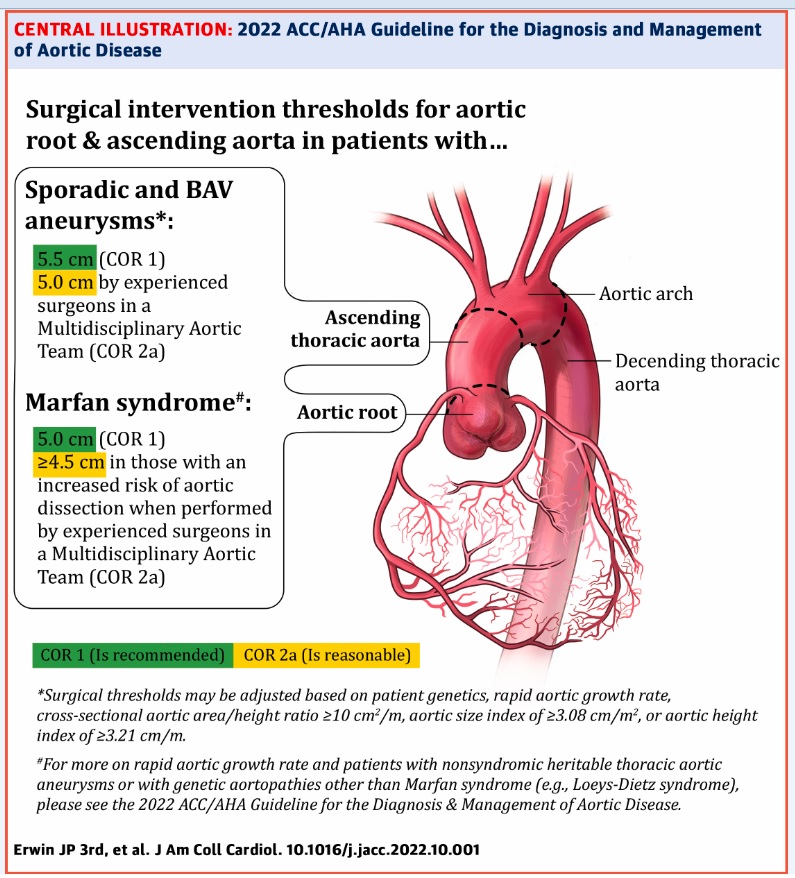
The 10 most important messages for the diagnosis and treatment of aortic disease 1. Because outcomes for patients with aortic disease improve in programs with higher volumes, experienced physicians, and extensive management capabilities, multidisciplinary aortic team care is considered to determine appropriate timing of intervention. 2. Shared decision making involving the patient and a multidisciplinary team is strongly recommended to determine optimal medical, endovascular, and open surgical therapies. In patients with aortic disease who are contemplating pregnancy or who are pregnant, shared decision-making is especially important when considering the cardiovascular risks of pregnancy, diameter thresholds for prophylactic aortic surgery, and mode of delivery. 3. Computed tomography, magnetic resonance imaging, and echocardiographic imaging of patients with aortic disease should follow recommended approaches for image acquisition, measurement and reporting of relevant aortic dimensions, and frequency of surveillance before and after the intervention. 4. In centers with multidisciplinary aortic teams and experienced surgeons, the threshold for surgical intervention for sporadic aortic root and ascending aortic aneurysms has been reduced from 5.5 cm to 5.0 cm in selected patients, and even lower in specific scenarios among patients with hereditary thoracic aortic aneurysms. 5. In patients who are significantly smaller or taller than average, surgical thresholds may incorporate indexing the aortic root or ascending aorta diameter to body surface area or patient height, or cross-sectional area aorta at the height of the patient. 6. Rapid aortic root growth or ascending aortic aneurysm growth, an indication for intervention, is defined as ≥0.5 cm in 1 year or ≥0.3 cm per year in 2 consecutive years for those with sporadic aneurysms and ≥0.3 cm in 1 year for those with hereditary disease of the thoracic aorta or bicuspid aortic valve. 7. In patients undergoing aortic root replacement surgery, valve-sparing aortic root replacement is reasonable if the valve is suitable for repair and when performed by experienced surgeons on a multidisciplinary aortic team. . 8. Patients with acute type A aortic dissection, if clinically stable, should be considered for transfer to a high-volume aortic center to improve survival. Surgical repair of type A aortic dissection should involve at least an open distal anastomosis rather than a simple supracoronary interposition graft. 9. There is an increasing role for thoracic endovascular aortic repair in the treatment of uncomplicated type B aortic dissection. Clinical trials of thoraco-abdominal aortic aneurysm repair with endoprostheses are reporting results that suggest that endovascular repair is an option for patients with adequate anatomy. 10. In patients with aortic root or ascending aorta aneurysms, or those with aortic dissection, screening of first-degree relatives with aortic imaging is recommended. |
Preamble
Since 1980, the American College of Cardiology (ACC) and the American Heart Association (AHA) have translated scientific evidence into clinical practice guidelines with recommendations to improve cardiovascular health. These guidelines, which are based on systematic methods for evaluating and classifying evidence, provide a foundation for the provision of quality cardiovascular care. The ACC and AHA sponsor the development and publication of clinical practice guidelines without commercial support, and members volunteer their time for writing and review efforts. The guidelines are official ACC and AHA policy.
For some guidelines, the ACC and AHA collaborate with other organizations. Intended Use Clinical practice guidelines provide recommendations applicable to patients with or at risk of developing cardiovascular diseases. The focus is on medical practice in the United States, but these guidelines are relevant to patients around the world. While the guidelines may be used to inform regulatory or payer decisions, the intent is to improve the quality of care and align with patient interests. The guidelines are intended to define practices that meet patients’ needs in most, but not all, circumstances and should not replace clinical judgment.
Clinical implementation
Management, according to guideline recommendations, is effective only when followed by both physicians and patients. Adherence to recommendations can be improved through shared decision-making between clinicians and patients, with patients involved in selecting interventions based on individual values, preferences, and associated conditions and comorbidities.
Comments
The American College of Cardiology and the American Heart Association released a new guideline on the diagnosis and treatment of aortic disease, which focuses on surgical intervention considerations, consistent imaging practices, genetic and familial screening, and the importance of a multidisciplinary aortic team.
The aorta is the largest artery in the body and carries oxygen-rich blood from the heart to the rest of the body. Aortic disease occurs when the aortic wall weakens and bulges, causing an aortic aneurysm, or tears, causing an aortic dissection. A ruptured aneurysm or severe dissection can be immediately fatal. If either is discovered through imaging tests, life-saving treatment may include careful monitoring of the injured aorta, surgery, medications, and/or lifestyle changes. Symptoms of aortic disease include chest pain or pressure, back pain, fatigue, neck pain, or jaw pain.
“There has been a tremendous amount of new evidence-based research available to clinicians over the past decade when it comes to aortic disease. It was time to reevaluate and update the previous existing guidelines,” said Eric M. Isselbacher, MD, MSc, chair of the guideline writing committee. “We hope that this new guideline can inform clinical practices with updated and summarized recommendations, aimed at a comprehensive multidisciplinary aortic team working to provide the best possible care to this vulnerable patient population.”
Recommendations in the new guide include:
Family evaluation : To identify people at increased risk for aortic disease, the new guideline recommends family evaluation, including genetic testing and imaging, of first-degree relatives of people diagnosed with aortic root or aortic aneurysms ascending thoracic, or those with aortic dissection. .
Imaging consistency – The guideline highlights the importance of consistency in how CT or MR images are obtained and reported, in measuring the size and characteristics of the aorta, and in how frequently They use the images to monitor before and after repair surgery or other intervention. Ideally, all surveillance imaging of a patient should be performed with the same modality and in the same laboratory.
Patient size adjustments : The guideline recommends modifying surgical thresholds in patients who are significantly smaller or taller than average. The guideline for the size of the aortic lesion that would indicate the need for surgery should be adjusted for the patient’s body surface area or height.
Surgery : In institutions with multidisciplinary aortic teams and experienced surgeons, the threshold for surgical intervention for sporadic aortic root and ascending aortic aneurysms has been lowered from 5.5 cm to 5.0 cm in certain individuals. The risk of aortic aneurysm or dissection increases with size. With this recommendation, selected people can undergo life-saving surgery sooner to avoid death from an aortic aneurysm or dissection.
Additionally, the guideline updates the definition of rapid aneurysm growth rate : surgery is recommended for people with aortic root and ascending thoracic aortic aneurysms with a confirmed growth rate of ≥0.3 cm per year for two years consecutive or ≥0.5 cm in one year. Rapid aortic growth is a risk factor for rupture.
Multidisciplinary aortic teams – For people requiring aortic intervention, outcomes are optimized when the surgery is performed by an experienced surgeon working on a multidisciplinary aortic team. The new guideline recommends “a specialized hospital team with experience in the evaluation and management of aortic disease, in which care is provided in a comprehensive and multidisciplinary manner.” These teams may be composed of cardiac and vascular surgeons with extensive experience managing complex aortic diseases in a center with a high volume of aortic interventions; imaging specialists with experience in aortic diseases who can interpret CT scans, MRIs, and echocardiograms; anesthesiologists with experience in the management of acute aortic disease and cerebrospinal fluid drainage; and an intensive care unit with experience in the management of acute aortic disease.
Shared decision making : The multidisciplinary aortic team is strongly encouraged to involve the patient in decision making, especially when individuals are borderline thresholds for repair or eligible for different types of surgical repair. Shared decision making should also be used with people who are pregnant or may become pregnant to consider the risks of pregnancy in people with aortic disease. Shared decision making has become increasingly important in patient-centered care and can be especially helpful when discussing quality of life, goals of care, and desired outcomes of the procedure.
This new guideline on aortic disease replaces the 2010 “ACCF/AHA Guidelines for the Diagnosis and Treatment of Patients with Thoracic Aortic Disease” and the 2015 “Surgery for Aortic Dilation in Patients With Bicuspid Aortic Valves: A ACC/AHA Task Clarification Statement Validity of Clinical Practice Guidelines.” It is intended to be used concurrently with the “2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease.” The new guideline brings together guidelines for the thoracic and abdominal aorta and is intended for cardiovascular physicians involved in the care of people with aortic disease, including general cardiovascular care physicians and emergency physicians.
The “2022 ACC/AHA Guideline for the Diagnosis and Treatment of Aortic Disease” will be published simultaneously in the Journal of the American College of Cardiology and in the journal Circulation of the American Heart Association. The guideline was collaboratively developed and endorsed by the American Association for Thoracic Surgery, the American College of Radiology, the Society of Cardiovascular Anesthesiologists, the Society for Cardiovascular Angiography and Interventions, the Society of Thoracic Surgeons, and the Society for Vascular Medicine. It was endorsed by the Society of Interventional Radiology and the Society of Vascular Surgery.