Out-of-hospital cardiac arrest accounts for more than 350,000 unexpected deaths each year in North America; Nearly 100,000 of these cardiac arrests are attributed to ventricular fibrillation or pulseless ventricular tachycardia. Patients with ventricular fibrillation or pulseless ventricular tachycardia have a higher survival rate than patients with other rhythms.
However, despite advances in defibrillator technology, nearly half of these patients may remain in refractory ventricular fibrillation despite multiple defibrillation attempts. In these patients, additional defibrillation without modifying the defibrillation method is usually not successful . Although antiarrhythmic medications such as amiodarone and lidocaine have been used to prevent refibrillation, neither has been definitively shown to improve survival to hospital discharge or neurologically intact survival.
Double sequential external defibrillation ( DSED), the technique of delivering rapid sequential shocks from two defibrillators with defibrillation pads placed in two different planes (anterior-lateral and anterior-posterior), has been studied for decades in the electrophysiology laboratory for its Use in patients with refractory atrial or ventricular fibrillation.
Vector switch (VC) defibrillation , the technique of changing the defibrillation pads from the anterior-lateral to the anterior-posterior position, offers the theoretical potential to defibrillate a portion of the ventricle that may not be completely defibrillated by the pads in the standard anterior-posterior position.
The use of DSED and CV defibrillation in out-of-hospital settings has been described in case reports, observational studies, and systematic reviews. These reports describe cases or series in which DSED was used as a last resort therapeutic option for patients who remained in refractory ventricular fibrillation, so these studies may have been confounded by resuscitation time bias or late application of a strategy. of defibrillation in a subgroup of patients for whom a positive result was unlikely.
It has been suggested that early application of DSED may be associated with higher rates of termination of ventricular fibrillation and return of spontaneous circulation than standard defibrillation. 13The objective of this trial (Double Sequential External Defibrillation for Refractory Ventricular Fibrillation [DOSE VF]) was to evaluate DSED and VC defibrillation compared to standard defibrillation in patients who remain in refractory ventricular fibrillation during out-of-hospital cardiac arrest.
Background
Despite advances in defibrillation technology, shock-refractory ventricular fibrillation remains common during out-of-hospital cardiac arrest. Double sequential external defibrillation (DSED; rapid sequential shocks from two defibrillators) and vector switch (VC) defibrillation (switching the defibrillation pads to an anteroposterior position) have been proposed as defibrillation strategies to improve outcomes in patients with refractory ventricular fibrillation.
Methods
We conducted a cluster-randomized crossover trial among six Canadian paramedic services to evaluate DSED and VC defibrillation compared with standard defibrillation in adult patients with refractory ventricular fibrillation during out-of-hospital cardiac arrest.
Patients were treated with one of these three techniques according to the strategy randomly assigned to the paramedic service.
The primary outcome was survival to hospital discharge.
Secondary outcomes included termination of ventricular fibrillation, return of spontaneous circulation, and good neurological outcome, defined as a modified Rankin Scale score of 2 or less (indicating no symptoms or mild disability) at hospital discharge. .
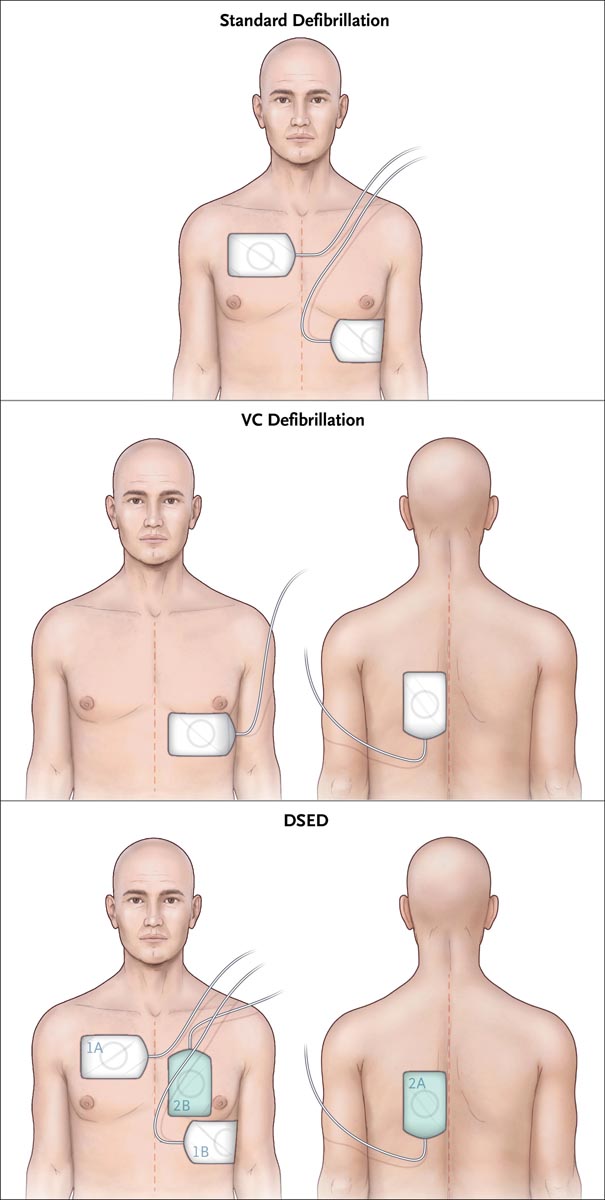
Electrode placement in the three defibrillation strategies . Location of patches for standard defibrillation, vector switch defibrillation (VC), and dual sequential external defibrillation (DSED) are shown. In the bottom panel, defibrillation pads 2A and 2B are those of the second defibrillator, with the pads placed in the posterior and anterior positions. For all strategies, the first three shocks occurred with pads placed in the configuration used for standard defibrillation.
Results
A total of 405 patients were enrolled before the data and safety monitoring board stopped the trial due to the coronavirus disease 2019 pandemic. A total of 136 patients (33.6%) were assigned to receive standard defibrillation, 144 (35.6%) to receive VC defibrillation and 125 (30.9%) to receive DSED.
Survival to hospital discharge was more common in the DSED group than in the standard group (30.4% vs. 13.3%; relative risk, 2.21; 95% confidence interval [CI], 1.33 to 3.67) and more common in the VC group than in the standard group (21.7% vs 13.3%; relative risk, 1.71; 95% CI, 1.01 to 2.88).
DSED defibrillation, but not VC , was associated with a higher percentage of patients with a good neurological outcome than standard defibrillation (relative risk, 2.21 [95% CI, 1.26 to 3.88] and 1. 48 [95% CI, 0.81 to 2.71], respectively).
Conclusions
Among patients with refractory ventricular fibrillation, survival to hospital discharge was more common among those who received DSED or VC defibrillation than among those who received standard defibrillation.
Discussion
In this randomized controlled trial of DSED or VC defibrillation for the treatment of refractory ventricular fibrillation during out-of-hospital cardiac arrest, survival to hospital discharge was more common among patients who received DSED or VC defibrillation than among those who received standard defibrillation . Termination of ventricular fibrillation, return of spontaneous circulation, and a good neurological outcome at hospital discharge appeared to be more common with the DSED strategy, as was termination of ventricular fibrillation with the VC defibrillation strategy.
The three groups appeared to be well matched in terms of timing of drug administration and mean doses of epinephrine and antiarrhythmic drugs administered, making an alternative therapeutic explanation for the trial findings unlikely. Although the results favored DSED, the logistics of having a second defibrillator available can be a challenge in some paramedic services. Since survival appeared to be higher with VC defibrillation than with standard defibrillation, the use of VC defibrillation with single-defibrillator systems may be an alternative therapeutic strategy for refractory ventricular fibrillation during out-of-hospital cardiac arrest when a second defibrillator.
Our findings contrast with those of previously reported observational studies and systematic reviews that have shown no benefit of DSED or VC defibrillation compared with standard defibrillation for patients who have had an out-of-hospital cardiac arrest. However, these studies lacked a control group with standard care characterized by high-quality CPR, did not control the timing of interventional shocks, did not describe a consistent technique for performing DSED or CV defibrillation, and did not measure or report the quality of CPR performed during DSED or VC defibrillation.
Survival to hospital discharge appeared to be higher with DSED and CV defibrillation than with standard defibrillation among patients with refractory ventricular fibrillation during out-of-hospital cardiac arrest.
(Funded by the Heart and Stroke Foundation of Canada; DOSE VF ClinicalTrials.gov number, NCT04080986. opens in new tab.)
Source : Defibrillation Strategies for Refractory Ventricular Fibrillation. Sheldon Cheskes, P. Richard Verbeek, Ian R. Drennan, Shelley L. McLeod, et al. NEJM DOI: 10.1056/NEJMoa2207304















