Early Active Mobilization during Mechanical Ventilation in the ICU
Background
Intensive care unit (ICU)-acquired weakness often develops in patients undergoing invasive mechanical ventilation. Early active mobilization can mitigate ICU-acquired weakness, increase survival, and reduce disability.
Methods
We randomly assigned 750 adult ICU patients who were receiving invasive mechanical ventilation to receive increased early mobilization (minimization of sedation and daily physical therapy) or usual care (the level of mobilization typically provided in each ICU).
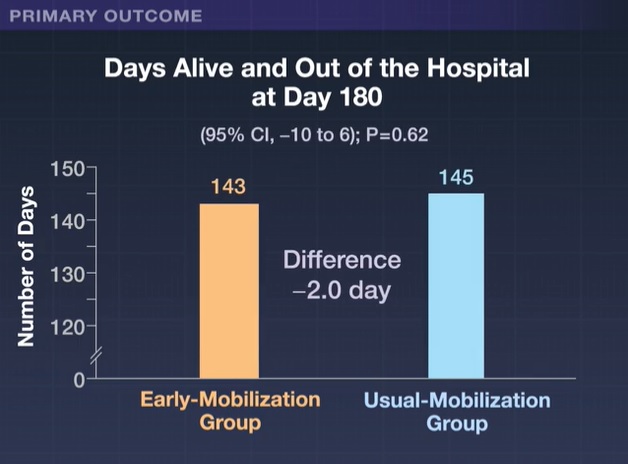
The primary outcome was the number of days patients were alive and out of the hospital at 180 days after randomization.
Results
The median number of days patients were alive and out of the hospital was 143 (interquartile range, 21 to 161) in the early mobilization group and 145 days (interquartile range, 51 to 164) in the usual care group (absolute difference, −2.0 days; 95% confidence interval [CI], −10 to 6; P = 0.62).
The mean (±SD) daily duration of active mobilization was 20.8±14.6 minutes and 8.8±9.0 minutes in the two groups, respectively (difference, 12.0 minutes per day; 95% CI). %, 10.4 to 13.6).
A total of 77% of patients in both groups were able to stand for a mean interval of 3 days and 5 days, respectively (difference, -2 days; 95% CI, -3.4 to -0.6). By day 180, death had occurred in 22.5% of patients in the early mobilization group and 19.5% of those in the usual care group (odds ratio, 1.15; 95% CI). 0.81 to 1.65).
Among survivors, quality of life, activities of daily living, disability, cognitive function, and psychological function were similar in the two groups.
Serious adverse events were reported in 7 patients in the early mobilization group and 1 patient in the usual care group. Adverse events possibly due to mobilization (arrhythmias, altered blood pressure, and desaturation) were reported in 34 of 371 patients (9.2%) in the early mobilization group and in 15 of 370 patients (4.1%) in the usual care group. group (P=0.005).
Conclusions
|
(Funded by the National Health and Medical Research Council of Australia and the Health Research Council of New Zealand; TEAM ClinicalTrials.gov number, NCT03133377. opens in new tab.)















