Most countries are falling behind in their commitments to the 2030 UN Sustainable Development Goal (SDG) of reducing premature mortality from non-communicable diseases (NCDs) by one third, the leading cause of death and poor health. Worldwide. Also of concern is the growing global burden of mental health problems, exacerbated by the COVID-19 pandemic.
At this rate, countries are unlikely to achieve their SDG 3 commitments by 2030 to ensure healthy lives and promote well-being for all at all ages.
Reducing the prevalence of modifiable risk factors , such as tobacco use, harmful alcohol use, unhealthy diets and physical inactivity, is a cost-effective strategy to reduce the burden of NCDs and mental health problems. Every US$1 invested in scaling up effective interventions to reduce risk factors and manage NCDs, for example, could generate a return of up to US$7 in low- and middle-income countries (LMICs), where almost 85% of all Premature deaths due to NCDs occur every year.
However, slow progress has been observed over the years, especially in such settings.
Physical inactivity is an important modifiable risk factor for NCDs and mental health conditions, including stroke, hypertension, type 2 diabetes, coronary heart disease, several types of cancer, dementia, depression and mortality for all causes; in particular, deaths from cardiovascular diseases.
The overall costs of physical inactivity to health care systems, based on just five health outcomes (coronary heart disease, stroke, type 2 diabetes mellitus, breast cancer, and colon cancer), were estimated in INT $53.8 billion (2013), of which 58% was paid by the public sector.
To support country responses, WHO identified 20 evidence-based policy recommendations, outlined in the WHO Global Action Plan on Physical Activity 2018-30, to guide national efforts to increase physical activity levels in people. population. But overall progress in reducing levels of physical inactivity has been slow.
Stronger advocacy is needed to establish the multisectoral action needed to promote and enable more physical activity. This advocacy can be supported by an economic case for governments and non-governmental organizations to invest in physical activity.
Summary
Background
Physical inactivity is an important modifiable risk factor for non-communicable diseases (NCDs) and mental health conditions. Our goal was to estimate the public health care costs associated with these diseases due to physical inactivity, which will help policymakers prioritize investment in policy actions to promote and enable more people to be more active.
Methods
We used a population attributable fraction formula to estimate the direct public healthcare costs of NCDs and mental health conditions for 2020–30. The disease outcomes we included were incident cases of coronary heart disease, stroke, type 2 diabetes, hypertension, cancer (breast, colon, bladder, endometrium, esophagus, gastric, and kidney), dementia, and depression in adults at least 18 years old. years. We use the most recent health and economic data evidence available for 194 countries.
Results
If the prevalence of physical inactivity does not change , there would be 499.2 million new cases of preventable serious non-communicable diseases worldwide by 2030, with direct healthcare costs of INT$520 billion.
The global cost of inaction on physical inactivity would reach approximately $47.6 billion per year. Although 74% of new NCD cases would occur in low- and middle-income countries, high-income countries would bear a greater proportion (63%) of the economic costs.
The cost of treating and managing NCDs varied: although dementia accounted for only 3% of new preventable NCDs, the disease accounted for 22% of all costs; type 2 diabetes accounted for 2% of new preventable cases but 9% of all costs; and cancers accounted for 1% of new preventable cases but 15% of all costs.
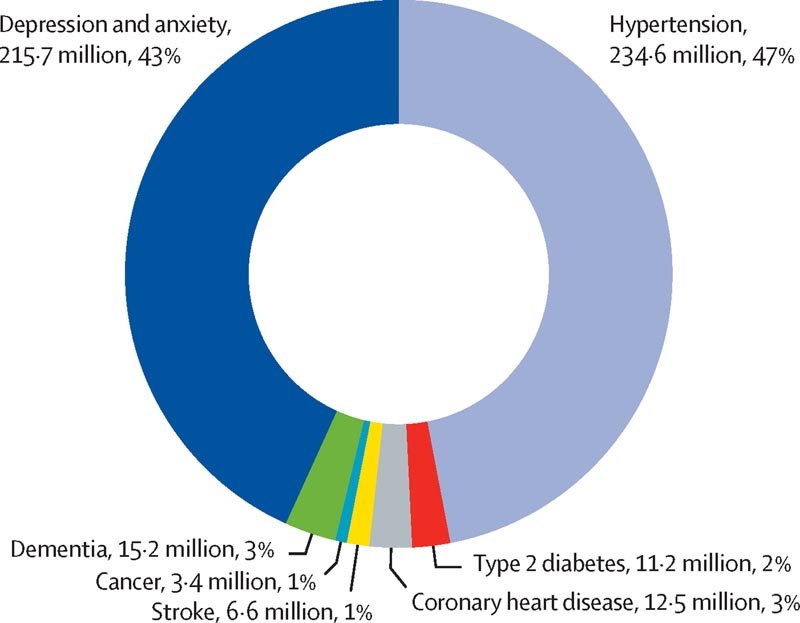
Figure: Total global number and proportion of new cases of non-communicable diseases and mental health conditions attributed to physical inactivity, 2020–30
Interpretation
This health and economic burden of physical inactivity is avoidable. Additional investments and implementation of known and effective policy interventions will help countries achieve the Sustainable Development Goal of reducing NCD mortality by 2030.
Research in context Evidence before this study Physical inactivity increases the risk of death from non-communicable diseases (NCDs). Only one previous global study estimated the direct healthcare costs resulting from physical inactivity using a disease prevalence-based approach, reporting an economic cost to society of INT$53.8 billion (2013 prices ), of which 58% was paid by the public sector. That study included five health outcomes for which relative risk estimates were available at that time. However, the study did not address the important questions of what potential current and future preventable public health care costs could be avoided if levels of physical inactivity were reduced or eliminated. Added value of this study This is the first global study to provide estimates of the number of new cases and associated public healthcare costs that would occur between 2020 and 2030 and that could be prevented if levels of physical inactivity were reduced or eliminated. This study provides new population attributable fractions for seven health outcomes and mental health conditions (coronary heart disease, stroke, type 2 diabetes, cancers [breast, colon, bladder, endometrial, gastric, esophageal and renal], depression and dementia) with strong evidence of the association with physical inactivity. Implications of all available evidence This study combines assessment of the health and economic impacts of NCDs and mental health conditions associated with physical inactivity, and provides policymakers with empirical data on the cost of not acting to reduce physical inactivity. . These data will equip policymakers with evidence to inform and advocate for greater investment in policy interventions that increase physical activity levels. This study calls for countries to take urgent action to prioritize investments in interventions that reduce this modifiable risk factor. The WHO Global Action Plan on Physical Activity provides clear guidance on evidence-based policy recommendations that, if implemented by countries, will improve health, reduce the burden on health systems and save money. |















