|
The 99th percentile of cardiac troponin, derived from a healthy reference population, is recommended as a diagnostic threshold for myocardial infarction, but troponin concentrations are strongly influenced by age. Our objective was to evaluate the diagnostic performance of cardiac troponin in older patients with suspected myocardial infarction.
In a secondary analysis of a multicenter trial of consecutive patients with suspected myocardial infarction, we evaluated the diagnostic accuracy of high-sensitivity cardiac troponin I at presentation for the diagnosis of type 1, type 2, or type 4b myocardial infarction in 3 age groups (<50, 50–74, and ≥75 years) using the age-adjusted and sex-specific 99th percentile thresholds recommended by the guidelines.
In 46,435 consecutive patients aged 18 to 108 years (mean, 61±17 years), 5216 (11%) had a diagnosis of myocardial infarction. In patients <50 (n=12,379), 50 to 74 (n=22,380), and ≥75 (n=11,676) years, the sensitivity of the guideline-recommended threshold was similar at 79.2% (95% CI). %, 75.5–82.9), 80.6% (95% CI, 79.2–82.1), and 81.6% (95% CI, 79.8–83.2), respectively.
Specificity decreased with advancing age from 98.3% (95% CI, 98.1–98.5) to 95.5% (95% CI, 95.2–95.8) and 82.6% (95% CI, 95.2–95.8) . 95%, 81.9–83.4).
Use of age-adjusted 99th percentile thresholds improved specificity (91.3% [90.8%–91.9%] versus 82.6% [95% CI, 81.9%–83.4%]). and positive predictive value (59.3% [57.0%–61.5%]] vs 51.5% [49.9%–53.3%]) for myocardial infarction in patients ≥75 years of age , but failed to prevent the decline of any of the parameters with increasing age and resulted in a marked reduction in sensitivity compared to using the guideline-recommended threshold (55.9% [53.6%–57 .9%] versus 81.6% [79.8%–83.3%].
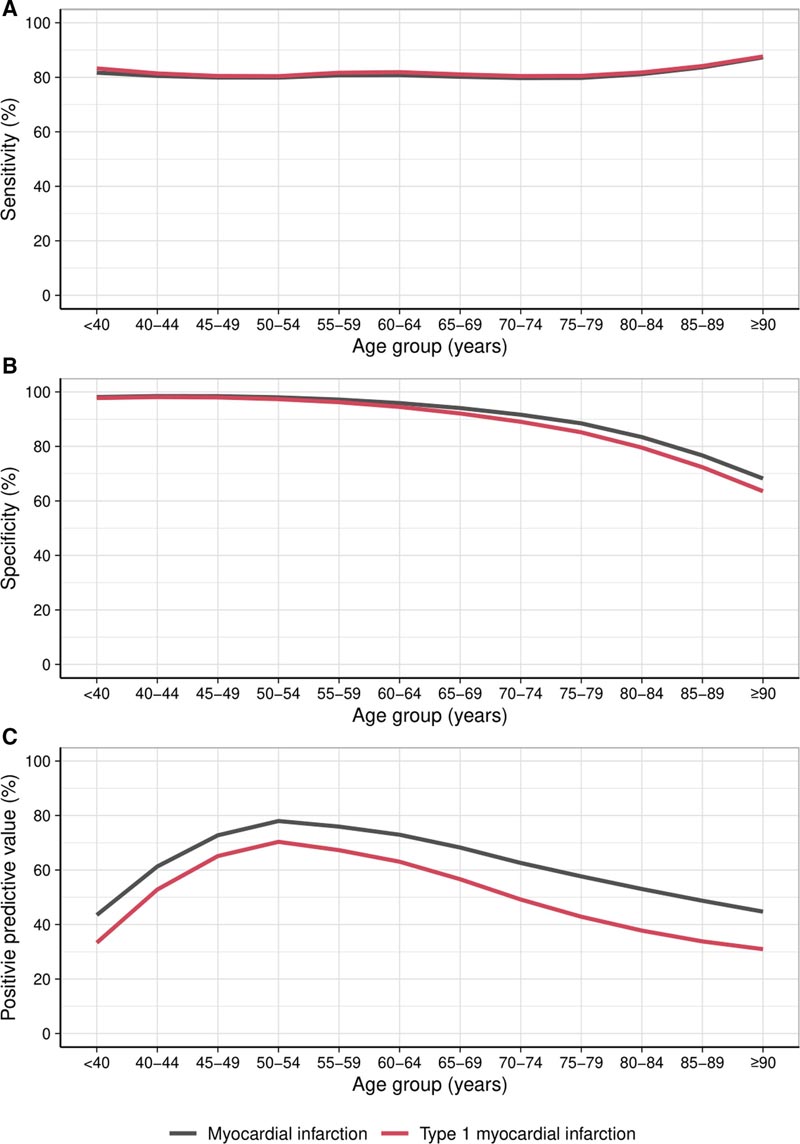
Diagnostic performance of the sex-specific 99th percentile for the diagnosis of myocardial infarction type 1. The sensitivity (A), specificity (B), and positive predictive value (C) of the recommended sex-specific 99th percentile for the diagnosis of myocardial infarction type 1 myocardium (red) compared to any myocardial infarction (black) represented with a line of best fit.
Age alters the diagnostic performance of cardiac troponin, with reduced specificity and positive predictive value in older patients when the guideline-recommended or age-adjusted 99th percentiles are applied. Individualized diagnostic approaches are needed rather than setting binary thresholds in an aging population.
In older patients presenting with suspected myocardial infarction, most cardiac troponin elevations are explained by acute or chronic myocardial injury or type 2 myocardial infarction.
The specificity and positive predictive value of high-sensitivity cardiac troponin in identifying myocardial infarction decreases with age and is observed if sex-specific or age-adjusted 99th percentile diagnostic thresholds or a "rule of thumb" threshold are applied. entry" for the triage of discharged patients. probability of myocardial infarction.
Serial troponin testing incorporating an absolute change in troponin concentration increased discrimination of myocardial infarction in older patients.
In older patients presenting with suspected myocardial infarction, clinicians should use caution when interpreting a single troponin measurement.
Clinicians should routinely perform serial measurements of cardiac troponin and consider absolute changes in concentration to identify those older patients with elevated troponin concentrations who are more likely to suffer a myocardial infarction.

The specificity and positive predictive value of high-sensitivity cardiac troponin decreases with age. It is recommended to use serial determinations.
For many years, some have advocated for using a higher cutoff value to diagnose older people with possible acute myocardial infarction (MI). The reason for this defense has been that it is well known that older people have higher cardiac troponin values. Some have argued that this is part of normal aging, while others have suggested that the etiology is due to comorbidities that develop over time.
Regardless of the etiology, elevated values in older people will reduce the specificity of cardiac troponin elevations for a diagnosis of myocardial infarction in the same way that other comorbidities such as kidney disease do, which is why the Universal Definition of Infarction of Myocardium advocates the use of a changing pattern of values to make the diagnosis. Others have worried that such an approach could inadvertently harm people who are older and healthy and therefore do not have high values.
The present evaluation by the Edinburgh group, High-STEACS Investigators , took advantage of the large number of patients they have studied to evaluate this issue. 46,435 patients between 18 and 108 years of age were included. The number with MI was 5216. “Specificity for the diagnosis of MI decreased with advancing age from 98.3% to 95.5% to 82.6%.
Use of age-adjusted 99th percentile thresholds improved specificity (91.3% vs. 82.6% and positive predictive value (59.3% vs. 51.5%) for myocardial infarction in patients ≥75 years, but failed to prevent the decline of any of the parameters with increasing age and resulted in a marked reduction in sensitivity compared to using the guideline-recommended threshold (55.9% vs. 81.6 %)”.
The message is clear and articulated by the authors in their clinical perspective. There are increases in cardiac troponin with age that negatively impact the specificity of the marker for the diagnosis of AMI. However, increasing the 99% URL as a way to address the problem significantly decreases the sensitivity of the diagnostic approach. For these reasons, the authors adopted the recommendations of the Universal Definition rather than using serial sample changes to help remedy this problem.
In conclusion , age has a significant effect on the diagnostic performance of cardiac troponin at the 99th percentile recommended by the guidelines for myocardial infarction, with reduced performance in older patients. The use of age-adjusted 99th percentile thresholds or a higher universal entry threshold did not achieve parity between middle-aged and older patients.
Individualized diagnostic approaches and serial testing are needed to determine the absolute change in troponin concentration rather than adjusting binary thresholds to avoid harming older patients.
















