Some people are known to age faster than others, some people live to old age without disease, while others develop age-related chronic diseases. With a rapidly aging population and an emerging epidemic of chronic diseases, finding mechanisms and implementing preventive measures that can slow down the aging process has become a new challenge for biomedical research and public health.
In mice , lifelong water restriction shortens lifespan and promotes degenerative changes. Here, we test the hypothesis that optimal hydration can slow the aging process in humans.
We performed a cohort analysis of data from the Atherosclerosis Risk in Communities study with middle-aged enrollment (45–66 years, n = 15,752) and 25 years of follow-up. We use serum sodium as an indicator of hydration habits. To estimate the relative speed of aging, we calculated biological age (BA) from age-dependent biomarkers and assessed the risks of chronic diseases and premature mortality.
The analysis showed that midlife serum sodium >142 mmol/L is associated with a 39% increased risk of developing chronic diseases (hazard ratio [HR] = 1.39, 95% confidence interval [CI] %: 1.18–1.63) and >144 mmol/l with an elevated risk of premature mortality of 21% (HR = 1.21, 95% CI: 1.02–1.45).
Individuals with serum sodium >142 mmol/L were up to 50% more likely to be older than their chronological age (OR = 1.50, 95% CI: 1.14–1.96). Higher BA was associated with a higher risk of chronic diseases (HR = 1.70, 95% CI: 1.50–1.93) and premature mortality (HR = 1.59, 95% CI 1.39–1 ,83).
People whose midlife serum sodium exceeds 142 mmol/l have a higher risk of being biologically older, developing chronic diseases, and dying at a younger age. Intervention studies are needed to confirm the link between hydration and aging.
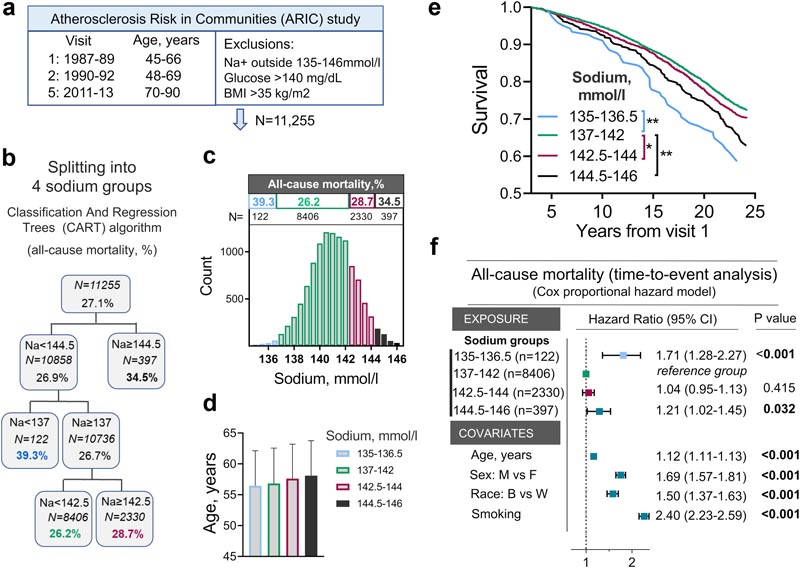
Fig. 1 Serum sodium in middle-aged people and risk of all-cause mortality in the Atherosclerosis Risk in Communities (ARIC) study. a) Summary of the ARIC study and exclusion criteria. b, c, d) Divide study participants into four groups using the classification and regression tree (CART) algorithm based on average serum sodium measured at visits 1 and 2 and cumulative mortality at the end of 25 years of follow up. b) Summary of the result of the CART algorithm for group division. c) Histograms showing the distributions of study participants according to serum sodium. The groups identified by the CART algorithm are shown in different colors. The mortality rate at the end of 25 years of follow-up and the number of people in each group are shown above the histogram. d) Average age does not differ between sodium groups. e, f) Assessment of the relative risk of all-cause mortality in four sodium groups. e) Kaplan-Meier survival analysis: P < 0.001 (log-rank test). All pairwise multiple comparison procedures): ∗P = 0.04, ∗∗P = 0.001 ( Holm-Sidak method). See Table S2 for N at risk at each time point. f) Time-to-event analysis: COX proportional hazards model. People whose middle-aged serum sodium exceeds 144 mmol/l or is less than 137 mmol/l have a higher risk of dying at a younger age. See also Table S2 for descriptive statistics and demographic data for these four sodium groups.
Adults who stay well hydrated appear to be healthier, develop fewer chronic conditions such as heart and lung disease, and live longer than those who do not get enough fluids, according to a National Institutes of Health study published in eBioMedicine .
Using health data collected from 11,255 adults over a 30-year period , researchers analyzed the links between serum sodium levels, which increase when fluid intake decreases, and several health indicators. They found that adults with serum sodium levels at the high end of a normal range were more likely to develop chronic diseases and show signs of advanced biological aging than those with serum sodium levels in the middle ranges. Adults with higher levels were also more likely to die at a younger age.
"The results suggest that adequate hydration can slow aging and prolong a disease-free life," said Natalia Dmitrieva, Ph.D., an author of the study and a researcher in the Laboratory of Cardiovascular Regenerative Medicine at National Heart University, the Lungs and Blood (NHLBI), part of the NIH.
The study expands on research that scientists published in March 2022, which found links between higher ranges of normal serum sodium levels and higher risks of heart failure. Both findings came from the Atherosclerosis Risk in Communities (ARIC) study, which includes substudies involving thousands of black and white adults across the United States. The first ARIC substudy began in 1987 and has helped researchers better understand the risk factors for heart disease while shaping clinical guidelines for its treatment and prevention.
For this latest analysis, the researchers evaluated the information that study participants shared during five medical visits: the first two when they were 50 years old and the last when they were between 70 and 90 years old. To allow a fair comparison between how hydration correlated with health outcomes, the researchers excluded adults who had high serum sodium levels at baseline checks or with underlying conditions, such as obesity, that could affect serum sodium levels. sodium.
They then assessed how serum sodium levels correlated with biological aging, which was assessed across 15 health markers. This included factors, such as systolic blood pressure, cholesterol and blood sugar, which provided information about how well each person’s cardiovascular, respiratory, metabolic, kidney and immune systems were functioning. They also adjusted for factors such as age, race, biological sex, smoking and hypertension.
They found that adults with higher levels of normal serum sodium, with normal ranges between 135 and 146 milliequivalents per liter (mEq/L), were more likely to show signs of faster biological aging. This was based on indicators such as metabolic and cardiovascular health, lung function and inflammation.
For example, adults with serum sodium levels greater than 142 mEq/L had an associated 10 to 15% increase in the odds of being biologically older than their chronological age compared to ranges between 137 and 142 mEq/L, while levels above 144 mEq/L correlated with a 50% increase. Likewise, levels of 144.5-146 mEq/L were associated with a 21% increased risk of premature death compared to ranges between 137-142 mEq/L.
Similarly, adults with serum sodium levels greater than 142 mEq/L had up to a 64% higher associated risk of developing chronic diseases such as heart failure, stroke, atrial fibrillation, and peripheral artery disease, as well as chronic lung disease, diabetes and dementia. In contrast, adults with serum sodium levels between 138 and 140 mEq/L had the lowest risk of developing chronic diseases.
The findings do not prove a causal effect, the researchers noted. Randomized controlled trials are needed to determine whether optimal hydration can promote healthy aging, prevent disease, and lead to longer life. However, associations can still inform clinical practice and guide personal health behavior.
“People whose serum sodium is 142 mEq/L or higher would benefit from an evaluation of their fluid intake,” Dmitrieva said.
He noted that most people can safely increase their fluid intake to reach recommended levels, which can be done with water and other fluids, such as juices or vegetables and fruits with high water content. The National Academies of Medicine, for example, suggests that most women consume about 6 to 9 glasses (1.5 to 2.2 liters) of fluids per day and for men, 8 to 12 glasses (2 to 3 liters).
Others may need medical guidance due to underlying health conditions. “The goal is to ensure that patients drink enough fluids, while evaluating factors, such as medications, that can lead to fluid loss,” said Manfred Boehm, MD, study author and director of the Cardiovascular Regenerative Medicine Laboratory. “Doctors may also need to defer a patient’s current treatment plan, such as limiting fluid intake for heart failure.”
The authors also cited research finding that about half of people worldwide do not meet recommendations for total daily water intake, which often starts at 6 cups (1.5 liters).
“Globally, this can have a big impact,” Dmitrieva said. “Decreased body water content is the most common factor that increases serum sodium, so the results suggest that staying well hydrated can slow the aging process and prevent or delay chronic diseases.” This research was supported by the NHLBI Internal Research Division. The ARIC study has been supported by research contracts from the NHLBI, NIH, and the Department of Health and Human Services.
In this study, we aimed to evaluate the pro-aging effects of mild subclinical hypohydration that activates water conservation mechanisms leading to the excretion of a smaller volume of more concentrated urine but does not elevate plasma sodium and osmolality more. beyond normal ranges.
We searched PubMed and Web of Science, without any language restrictions, using combinations of the terms “serum sodium”, “hydration”, “aging”, “biological aging”, “chronic diseases”, “mortality”. We focused on finding studies that evaluated associations between the hydration status of healthy middle-aged or younger people with long-term aging-related outcomes, such as future development of chronic diseases or premature mortality.
We were also looking for studies that estimated biological age in relation to markers of habitual low hydration such as serum sodium. We did not find studies that relate markers of subclinical hypohydration in middle age with the speed of biological aging. Several observational epidemiological studies have identified associations of hydration markers with the future development of heart failure, metabolic disease, and mortality. An increased risk of mortality after 3 to 6 years of follow-up was demonstrated among persons with serum sodium at the upper end of the normal range.
The current study presents a comprehensive analysis of a large population-based observational study with a long-term follow-up of 25 years .
The analysis demonstrated that midlife serum sodium at the upper part of the normal range (135–146 mmol/l) is able to predict a faster rate of biological aging and a greater burden of chronic diseases later in life, including heart failure, dementia, chronic lung disease, stroke, diabetes, peripheral vascular disease and atrial fibrillation.
The analysis identified a serum sodium threshold of 142 mmol/L that can be used in clinical practice to identify individuals at risk.
In this study, we report that serum sodium at the upper part of the normal range is a risk factor for accelerated aging. In the ARIC study, the odds of being biologically older than chronological age increased in study participants whose serum sodium exceeded 142 mmol/L , reaching a 50% increase in odds with sodium levels greater than 144 mmol/L . Such a high BA in middle age (47-68 years) translates into an approximately 20% increase in the risk of premature mortality with sodium levels above 144 mmol/l and an increased risk of developing chronic diseases, which was already evident at sodium concentrations above 140 mmol/l and increased risk approximately 40% in the 143–146 mmol/l group.
In addition to the elevated risk of mortality and chronic disease at the high end of the normal serum sodium range, an increased risk was also evident at the low end of the normal sodium range. This is consistent with previous reports of increased mortality and incidence of cardiovascular diseases (CVD) in community subjects with low normal sodium (135–137 mmol/L) that is attributed to diseases that cause electrolyte dysregulations.
Our results indicate that the serum sodium range between 138 and 142 mmol/l is associated with a lower risk of chronic diseases and/or premature mortality. This range corresponds to a more conservative definition of normal range proposed by Kumar and Berl.
Since decreased body water is the most common reason for increased sodium concentration, these results suggest that for people whose serum sodium exceeds 142 mmol/L, consistently maintaining optimal hydration may slow the aging process.
In summary , our study shows that people whose fasting serum sodium exceeds 142 mmol/l have a higher risk of being biologically older, developing chronic diseases and dying at a younger age. This threshold can be used in clinical practice to identify people at risk.
Since decreased hydration is one of the main factors that elevate serum sodium, the results are consistent with the hypothesis that decreased hydration may accelerate aging. However, intervention trials are needed to test this link. Global surveys find that more than 50% of people do not drink the recommended amounts of fluids.
Therefore, the results of our study provide additional reasons to reinforce already existing recommendations for optimal fluid intake. A strategy has recently been proposed to develop personal recommendations on optimal fluid intake based on health status.
The findings of this and previous studies are consistent with the hypothesis that decreased hydration may accelerate aging . The findings suggest that people whose serum sodium exceeds 142 mmol/L may benefit from more comprehensive clinical evaluation of their hydration status, including fluid intake habits and pathological conditions that may predispose to greater water loss. The results justify testing the potential anti-aging effects of improved hydration in intervention trials and support the addition of recommendations for optimal fluid intake to prevention guidelines.
This work was funded by the Intramural Research program of the National Heart, Lung, and Blood Institute (NHLBI). The ARIC study has been funded in whole or in part with federal funds from the NHLBI; the National Institutes of Health (NIH); and the Department of Health and Human Services.
















