Digoxin Use in Contemporary Heart Failure with Reduced Ejection Fraction: An Analysis of the Swedish Heart Failure Registry
Digoxin is included in some heart failure (HF) guidelines, but controversy persists about the true role and impact of treatment with this drug, particularly in the absence of atrial fibrillation (AF) .
The objective of this study was to evaluate the association between clinical characteristics and digoxin use and between digoxin use and mortality/morbidity in a large contemporary cohort of patients with HF with reduced ejection fraction (HFrEF) stratified by history of atrial fibrillation (AF).
Patients with HFrEF (EF < 40%) enrolled in the Swedish HF registry between 2005 and 2018 were analyzed. The independent association between digoxin use and patient characteristics was assessed using logistic regression, and between digoxin use and outcomes [composite of all-cause mortality or HF hospitalization (HFH), all-cause mortality, and HFH] using Cox regressions in a 1:1 propensity score-matched population.
Digoxin use was analyzed at baseline and as a time-dependent variable. Of 42,456 patients with HFrEF, 16% received digoxin, 29% in the AF group and 2.8% in the non-AF group.
The main independent predictors of use were advanced HF, elevated heart rate, history of AF, preserved renal function, and concomitant use of beta-blockers.
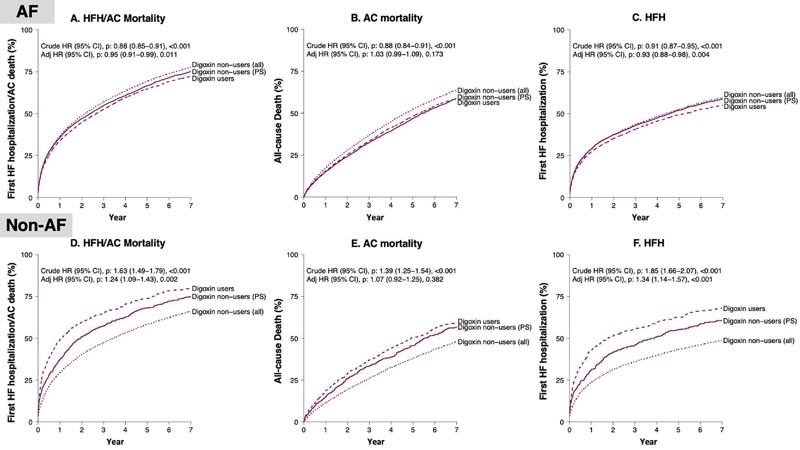
Digoxin use was associated with a lower risk of all-cause death/HFH [hazard ratio (HR): 0.95; 95% confidence interval (CI): 0.91-0.99] in patients with atrial fibrillation (AF), but with a higher risk in patients without AF (HR: 1.24; 95% CI: 1.09- 1.43). Consistent results were observed when digoxin use was analyzed as a time-dependent variable.
Associations between digoxin use and outcomes
In patients with HFrEF, overall digoxin use was modest and decreased over time, but was significantly higher in patients with atrial fibrillation (AF) than without AF.
Digoxin use was associated with a lower risk of death/HFH in patients with HFrEF and atrial fibrillation (AF), supporting current guideline recommendations, but was associated with an increased risk of adverse events in patients with HFrEF without atrial fibrillation (AF), which contrasts with the DIG randomized trial.
Given the observational design of the current study, which does not allow investigation of efficacy, our findings warrant confirmation in contemporary RCTs. However, our analysis adds important information on the current use of digoxin in clinical practice and its association with outcomes according to current indications, with important implications in terms of implementation of digoxin use, whether future RCTs can show that digoxin is effective or not.
















