We now have adequate data to describe the main symptoms, course and prevalence of long COVID which include shortness of breath, muscle pain, anosmia, tingling in the extremities and general fatigue. Many of these symptoms are non-specific, but are seen at higher rates in people with long COVID than would be expected in the general population.
Despite intense research in the area, no clear pathogenesis has been established that can explain the full range of long COVID symptoms.
Studies have found that patients’ symptoms in many cases persist beyond the point at which pathophysiological observations can adequately explain them.
Symptoms not adequately explained by traditional medical research paradigms are common throughout medicine and represent the most common diagnosis in some specialties.
Persistent symptoms are highly prevalent in the general population and even within well-defined disease cohorts, there is often little association between objective pathophysiology and symptom burden.
Coherent and relatable explanatory models are key to engaging patients with appropriate treatment and act as a model to guide research. This need for explanatory models in long COVID invites various responses.
- The first response is to continue the search for an all-encompassing pathophysiological mechanism .
- The second response is to pursue a personalized medicine approach through attempts to cluster clinical phenotypes.
- We propose a third response that allows for a more complex understanding of the reciprocal relationships between triggers, conditioning mechanisms, and symptoms.
Long COVID could be explained as an embodied condition with heterogeneous biological, psychological (experiential), and social (or environmental) factors embedded in complex relationships (figure).
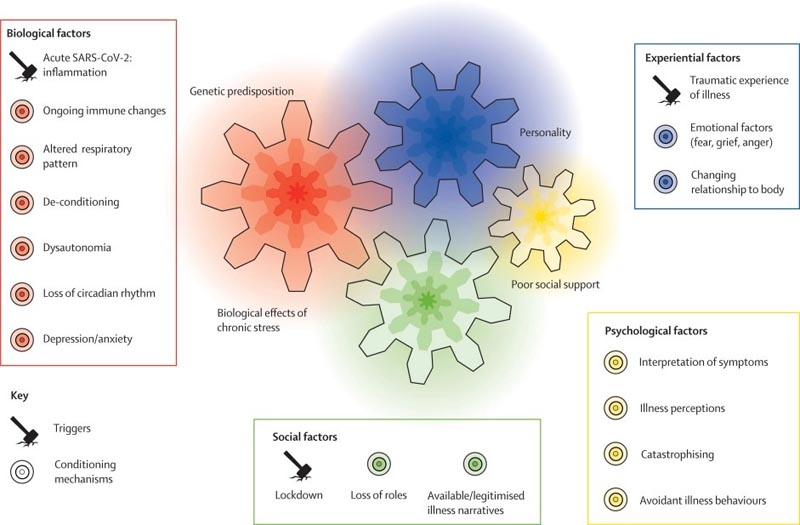
Causal model of interaction of biological, social, experiential and psychological factors in long COVID
These complex relationships in the generation and persistence of symptoms have been investigated most extensively by those working in the field of functional disorders .
Specific linear causal processes within organs and tissues cannot explain all physical suffering.
For some conditions, it is necessary to approach treatment holistically rather than on an individual pathophysiological basis. Effective treatments and rehabilitation approaches for functional disorders are known and many of them are already used in long COVID clinics. However, explicit explanatory models that address the need for multidisciplinary and integrated treatment provision are key to improved clinical services. Poorly integrated explanatory models contribute to poor care and stigma of people who are sick in these specific ways.
In summary, we welcome research into the cellular and physiological mechanisms behind persistent symptoms, including post-viral fatigue. However, it is increasingly clear that simple causal relationships between pathophysiology and symptoms inadequately explain many chronic diseases and health conditions, including long COVID.
There is a body of literature available on the multiple factors involved in the generation, perception and persistence of functional symptoms, and models through which to integrate them. We are moving into a new era in long COVID research and treatment that would benefit from an integrated paradigm through which to understand human disease. We suggest that it is time to break taboos based on a dualistic understanding of physical versus mental illness and incorporate existing knowledge about functional somatic symptoms to provide better explanations and treatments.