Background
Multimorbidity is common among patients with fractures. However, its association with osteoporosis research and treatment to prevent future fractures is unclear. This limited knowledge prevents optimal patient care.
This study investigated the association between multimorbidity and osteoporosis screening and treatment in high-risk individuals after an osteoporotic fracture.
Methods and findings
The Sax Institute’s 45 and Up study is a prospective, population-based cohort of 267,153 people in New South Wales, Australia, recruited between 2005 and 2009. This analysis followed participants until 2017 for a median of 6 years (IQR: 4 to 8).
Questionnaire data were linked to hospital admissions (Admitted Patient Data Collection (APDC)), emergency presentations (Emergency Department Data Collection (EDDC)), Pharmaceutical Benefits Scheme (PBS) and Medicare Benefits Schedule (MBS).
Data were linked by the Center for Health Record Linkage and stored in a secure computing environment. APDC and EDDC fractures, APDC Charlson Comorbidity Index (CCI), MBS dual-energy X-ray absorptiometry (DXA) investigation, and PBS osteoporosis treatment were identified.
Of 25,280 people with an index fracture, 10,540 were classified as high risk based on the 10-year Garvan fracture risk threshold (age, sex, weight, previous fracture, and falls) ≥20%. The association of CCI with the probability of investigation and initiation of treatment was determined using logistic regression adjusted for education, socioeconomic and lifestyle factors).
High-risk women and men averaged 77 ± 10 and 86 ± 5 years, respectively; >40% had a CCI ≥2. Only 17% of women and 7% of men received a DXA referral, and 22% of women and 14% of men received osteoporosis medication after a fracture.
A higher CCI was associated with a lower likelihood of being investigated [adjusted OR, women: 0.73 (95% CI, 0.61 to 0.87) and 0.43 (95% CI, 0.30 to 0. 62); men: 0.47 (95% CI, 0.33 to 0.68) and 0.52 (0.31 to 0.85) for ICC: 2 to 3 and ≥4 versus 0 to 1, respectively] and receiving osteoporosis medication [adjusted OR, women: 0.85 (95% CI, 0.74 to 0.98) and 0.78 (95% CI, 0.61 to 0.99); men: 0.75 (95% CI, 0.59 to 0.94) and 0.37 (95% CI, 0.23 to 0.53) for ICC: 2 to 3 and ≥ 4 versus 0 to 1, respectively ].
The cohort is relatively healthy; therefore, the impact of multimorbidity on osteoporosis treatment may have been underestimated.
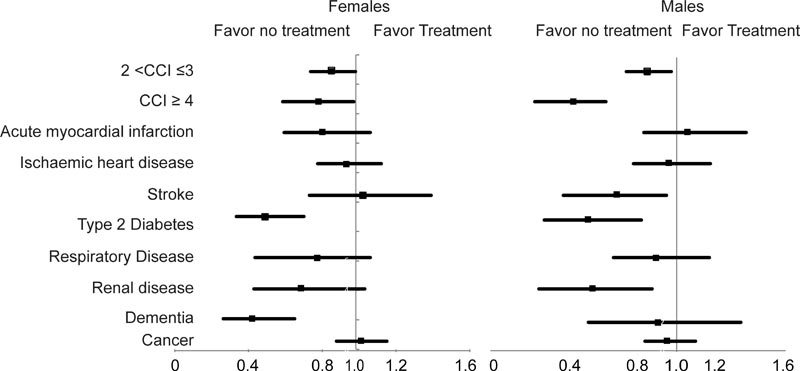
Association between chronic conditions and initiation of treatment in the high-risk group.
Conclusions
Multimorbidity contributed significantly to the osteoporosis treatment gap . This suggests that fracture risk is underestimated in the context of multimorbidity and highlights the need for additional surveillance and improved fracture care in this context.
Comments
Worse health outcomes for at-risk patients with fractures
Patients with complex medical conditions at high risk of fracture receive insufficient treatment for fracture prevention, but are at increased risk of further fractures.
The new study is published in the journal PLOS Medicine .
People at high risk of fracture who also have complex or multiple chronic medical conditions are less likely to receive treatment for underlying osteoporosis and also have worse health outcomes, according to a new study from the Garvan Institute of Medical Research.
These patients are at increased risk for additional fractures, but are less likely to have the underlying cause of the fracture investigated, compared to those at high risk but who do not have additional chronic conditions.
"No matter the site of the fracture, we believe that the fracture is not prioritized in the clinical setting in a complex patient," says lead author Dr. Dana Bliuc, senior research director in the Laboratory of Clinical Studies and Epidemiology at Garvan.
“People with complex diseases not only do worse, they are less likely to receive treatment, which is a double whammy. We believe this is because fractures are considered less serious than other medical conditions present in patients and are therefore not the focus of intervention,” says Dr. Bliuc. “But the fracture itself will affect quality of life and contribute to mortality.”
The findings will help inform new guidelines for how doctors investigate and treat fractures in patients with complex medical conditions.
Fractures from falls and mishaps, rather than traumas such as car accidents, occur in about one in three women and one in five men over the age of 50.
To investigate the outcomes and type of medical treatment people with these fractures receive, researchers studied the prescriptions, Medicare claims and hospital admission data of more than 10,500 Australian patients over 45 years of age, identified as high risk. of suffering a future fracture.
They found that in patients in the high-risk group, more than 80% of people did not receive treatment for osteoporosis to prevent future fractures, when they should have, and this decreased further for patients with complex medical conditions.
"We need to start changing our paradigm of how we think about illness and treatment so that it is less of a ’one illness-one treatment’, and we treat the person as a whole," says Professor Jacqueline Center, Head of Studies Clinical and Epidemiology Laboratory in Garvan.
“Our goal is to improve the health of older people, so that they live well, rather than just living.”
Why was this study done?
What did the researchers do and find?
What do these findings mean?
|
This research was supported by a competitive grant from Amgen and a NHMRC/MRFF Next Generation Clinical Investigator Program Professional Fellowship.
Professor Jacqueline Center is an Associate Professor at St Vincent’s Clinical School, Faculty of Medicine and Health, UNSW Sydney. Dr Dana Bliuc is a Senior Lecturer in the School of Population Health, Faculty of Medicine and Health, UNSW Sydney.















