An estimated 537 million adults aged 20 to 79 were living with diabetes worldwide in 2021, and more than 90% of them had type 2 diabetes. Type 2 diabetes is associated with an increased risk of several vascular complications, such as myocardial infarction, stroke, peripheral arterial disease and kidney disease, leading to premature death.
Previous studies have reported declining rates over the past two decades of major cardiovascular complications and mortality in people with diabetes in some high-income countries, with parallel larger contributions from other diseases, such as cancer, as underlying causes of death. In fact, accumulated epidemiological evidence has demonstrated an increased risk of incidence and mortality for some types of cancer in people with type 2 diabetes, with prolonged exposure to the effects of hyperglycemia , hyperinsulinemia, insulin resistance, and inflammation chronic factors underlying potential biological mechanisms. Strong evidence indicates that there is a causal relationship between type 2 diabetes and pancreatic, liver, and endometrial cancer; Both diabetes and cancer have also been linked to obesity and smoking.
While previous studies have extensively investigated inequalities in vascular outcomes among people with type 2 diabetes by sociodemographic factors, less is known about whether such inequalities exist in cancer mortality rates. Therefore, in this study we aimed to describe long-term trends in cancer mortality rates in people with type 2 diabetes based on subgroups defined by sociodemographic characteristics and risk factors.
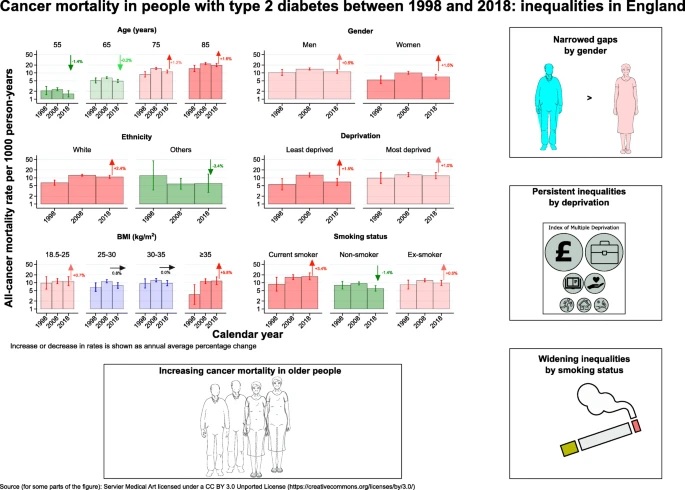
Summary Objectives/hypotheses The objective of this study was to describe long-term trends in cancer mortality rates in people with type 2 diabetes based on subgroups defined by sociodemographic characteristics and risk factors. Methods We defined a cohort of people aged ≥35 years who had newly diagnosed type 2 diabetes in the Clinical Practice Research Datalink between January 1, 1998 and November 30, 2018. We assessed trends in all-cause mortality rates, by all cancer types and cancer-specific by age, sex, ethnicity, socioeconomic status, obesity and smoking. We used Poisson regression to estimate age- and calendar-year-specific mortality rates and Joinpoint regression to assess trends in each outcome. We estimated standardized mortality ratios by comparing mortality rates in people with type 2 diabetes with those in the general population. Results Among 137,804 people , over a median follow-up of 8.4 years , all-cause mortality rates decreased at all ages between 1998 and 2018; Cancer death rates also decreased for those ages 55 and 65, but increased for those ages 75 and 85, with average annual percentage changes (AAPC) of –1.4% (CI 95%: –1.5, –1.3), –0.2% (–0.3, –0.1), 1.2% (0.8, 1.6) and 1.6% ( 1.5, 1.7), respectively. Higher AAPCs were observed in women than in men (1.5% vs. 0.5%), in the least disadvantaged than in the most disadvantaged (1.5% vs. 1.0%), and in people with morbid obesity. than those with normal body weight (5.8% vs. 0.7%), although all of these stratified subgroups showed increasing trends in cancer mortality rates. Increasing rates of cancer mortality were also seen in white people and former/current smokers, but decreasing trends were seen in other ethnic groups and non-smokers. These results have led to persistent inequalities by gender and deprivation, but greater disparity by smoking status. Steady upward trends in mortality rates were also observed for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and prostate cancer. endometrium in older ages. Compared with the general population, people with type 2 diabetes had a more than 1.5 times higher risk of mortality from colorectal, pancreatic, liver, and endometrial cancer throughout the study period. Conclusions/interpretation In contrast to decreases in all-cause mortality rates at all ages, the burden of cancer has increased in older people with type 2 diabetes, especially for colorectal, pancreatic, liver, and endometrial cancer. Personalized cancer prevention and early detection strategies are needed to address persistent inequalities in the older population, the most disadvantaged and smokers. |
Comments
New research, funded by Hope Against Cancer and published in Diabetologia (the journal of the European Association for the Study of Diabetes [EASD]) shows that cancer mortality in people with type 2 diabetes is substantially higher than the general population, by 18% for all cancers combined, 9% for breast cancer and 2.4 times for colorectal cancer. Cancer mortality in people with diabetes was also about twice as high as in the general population for diabetes-related cancers, including cancers of the liver (both sexes), pancreas (both sexes), and endometrium (women only).
The study, conducted by Dr Suping Ling, the Leicester Real World Evidence Unit, the Leicester Diabetes Research Centre, the University of Leicester and the London School of Hygiene and Tropical Medicine, UK, also showed an increase in breast cancer mortality rates by 4.1% per year, in younger women. women with type 2 diabetes, during the 20-year study period from 1998 to 2018.
Accumulated epidemiological evidence has demonstrated an increased risk of incidence and mortality for some types of cancer in people with type 2 diabetes, with prolonged exposure to the effects of increased blood sugar and insulin levels, with insulin resistance being and chronic inflammation the possible underlying biological mechanisms. Strong evidence indicates that there is a causal relationship between type 2 diabetes and pancreatic, liver and endometrial cancer. While previous studies have extensively investigated disparities in cardiovascular outcomes among people with type 2 diabetes, less is known about whether such disparities exist in cancer mortality rates.
In this study, the authors used a cohort of people aged 35 years or older who had newly diagnosed type 2 diabetes in Clinical Practice Research Datalink , a UK general practice database, over a 20-year period between 1 January 1998 and November 30, 2018. They analyzed trends in mortality rates from all causes, from all types of cancer, and from cancer specific to age, sex, ethnicity, socioeconomic status, obesity, and smoking. They also calculated standardized mortality rates by comparing death rates in people with type 2 diabetes to the general population.
The study included 137,804 people with newly diagnosed type 2 diabetes with a median follow-up of 8.4 years. The authors found that all-cause mortality rates decreased at all ages between 1998 and 2018; Cancer death rates (all cancers combined except non-melanoma skin cancer) also decreased for 55-year-olds (by 1.4% per year) and 65-year-olds (by 0.2% per year). year), but they increased for people aged 75 years (by 1.2% annually) and those aged 85 years (by 1.6% annually).
The authors say that the decline in cardiovascular mortality seen in older age groups, due to successful cardiovascular prevention and treatment in recent decades, means people are living longer now and are more likely to experience other conditions and, therefore, dying from other causes (including cancer). However, diabetes screening, better control of diabetes and its complications, early detection of cancer, and improved cancer treatments appear to have benefited younger people with T2D in the same way they have. done in the general population.
There were also higher “average annual percentage changes” (AAPC, the average percentage increase/decrease per year) in cancer mortality in women (1.5%) compared to men (1.0%), although women had lower cancer mortality throughout the study period. Biological factors, health-seeking behaviors, and lifestyle factors such as smoking and obesity differ between men and women, but the relative contribution of each to cancer mortality is unknown. The least disadvantaged/richest group also had a higher AAPC (1.5%) than the most disadvantaged/poorest group (1.0%), leading to a narrowing but persistent gap by socioeconomic status.
Other key findings included higher AAPC cancer mortality for people with morbid obesity (5.8%) compared to those in other weight categories (all below 1.0%), as well as higher AAPC cancer mortality for white people (2.4%) compared to an average annual percentage drop of 3.4% among non-white ethnicities combined. The gap in cancer mortality between smokers and non-smokers also increased, with smokers experiencing an increase in cancer mortality AAPC of 3.4%, while for non-smokers the AAPC decreased by 1.4%. The authors suggest that current health policies and structures could benefit never-smokers more than smokers, and that tailored interventions for smokers, such as targeted screening programs, could help address rising mortality from the disease. cancer (and all-cause mortality) in smokers.
Steady upward trends in mortality rates were also observed for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and prostate cancer. endometrium in older ages.
Breast cancer mortality rates in young women with T2D are increasing: authors suggest breast cancer screening could be extended to younger women with T2D
Compared with the general population, people with type 2 diabetes had a more than 1.5 times higher risk of mortality from colorectal, pancreatic, liver, and endometrial cancer throughout the study period. Despite national reports from this period showing a decrease in breast cancer mortality in the younger age ranges in this study, this new research also showed an increase in breast cancer mortality rates by 4 .1% per year in younger women with type 2 diabetes.
The authors suggest: “From this perspective, our results suggest that it may be useful to extend breast cancer screening to young women with type 2 diabetes. However, given the high cost and potentially longer exposure to screening procedures, Cost-effectiveness analyzes are required to define the appropriate time window and identify subgroups that may benefit most.” They add that there are currently trials investigating extending the existing breast cancer screening window from 50 to 70 years to 47 to 73 years in the general population; Additionally, women with a family history of breast cancer or specific genetic mutations are offered screening from a younger age, but no current guidelines specifically consider the increased risk of breast cancer in women with diabetes.
Regarding overall cancer mortality in people with diabetes, the authors say: “Prevention of cardiovascular disease has been, and still is, considered a priority in people with diabetes. Our results challenge this view by showing that cancer may have overtaken cardiovascular disease as the leading cause of death in people with type 2 diabetes. Therefore, cancer prevention strategies deserve at least a similar level of attention. for the prevention of cardiovascular diseases, particularly in older people and for some types of cancer, such as liver, colorectal and pancreatic cancer.
Tailored interventions should also be considered for smokers, who had higher and steadily increasing cancer mortality rates. Interventions for smokers, in addition to smoking cessation, could include campaigns to raise cancer awareness and improve early detection. For people with type 2 diabetes, early detection of cancer through changes to existing screening programs, or more in-depth investigations for suspicious or non-specific cancer symptoms, can reduce the number of preventable cancer deaths.”
The authors conclude: “In conclusion, our findings underscore the increasing burden of cancer in people with type 2 diabetes, particularly in older people, and highlight the need to prioritize prevention, research, and early detection and management of cancer in this age group.” population, especially for colorectal cancer, pancreatic, liver and endometrial cancer, whose mortality rates were substantially higher in people with type 2 diabetes than in the general population.
Final message These findings underline the increasing burden of cancer in people with type 2 diabetes, particularly in older people, and highlight the need to prioritize prevention, research and early detection and management of cancer in this population, especially for colorectal, pancreatic cancer , liver and endometrial cancer, whose mortality rates were substantially higher in people with type 2 diabetes than in the general population. Persistent inequalities in cancer mortality rates by sociodemographic factors and increasing disparities by smoking suggest that tailored cancer prevention and screening strategies are needed. For example, some subgroups, such as smokers, experienced not only higher mortality rates but also increasing mortality trends over the study period. |
















