Key points Ask Is there a robust and reproducible blood lipid profile characteristic of severe mental disorders? Findings In this diagnostic study including 1552 individuals, significant blood plasma lipidome alterations were identified that reproducibly and accurately separated individuals with schizophrenia from controls in 3 distinct population cohorts from China, Western Europe, and Russia. Parallel analysis of lipid alterations present in the blood plasma of people with major depressive disorder and bipolar disorder further revealed significant transdiagnostic overlap . Meaning The results of the study suggest that a shared profile of quantitative alterations in plasma lipids is characteristic of individuals from various populations affected by severe mental disorders. |
There is growing interest in the use of lipids as potential biomarkers of pathophysiological processes, particularly psychiatric disorders, where currently, to our knowledge, there are no clinically useful diagnostic tests. However, changes in serum and plasma lipid profiles have been repeatedly observed in patients with psychiatric diagnoses, mainly in small-scale studies. Clinical lipid measurements revealed an increase in triglyceride levels in individuals with schizophrenia (SCZ) who were receiving medication, those who were treatment-naïve, those with a first episode of psychosis, and individuals with prior major depressive disorder (MDD). of the treatment.
Nonclinical lipidomics studies examining a broader scope of lipid classes yielded repeated observations of decreased ether phospholipids in patients with SCZ and less consistent alterations of acylcarnitines. MDD studies also reported reduced levels of ether phospholipids and reduced levels of acylcarnitines. Furthermore, increased ceramide levels were reproducibly shown in both MDD and bipolar disorder (BPD) with specific ceramide species proposed as potential markers of depression.
Although these results demonstrate the potential of lipids as peripheral biological markers of psychiatric disorders, the existence of a reliable and specific signature of these disorders, sufficiently independent of demographic and environmental variables, remains unclear.
Importance
There is no clinically applicable diagnostic test for severe mental disorders. Lipids harbor potential as disease markers.
Aim
To define a reproducible profile of lipid alterations in the blood plasma of patients with schizophrenia (SCZ) independently of demographic and environmental variables and to investigate its specificity in association with other psychiatric disorders, i.e., major depressive disorder (MDD) and bipolar disorder. (DBP).
Design, environment and participants
This was a multi-cohort case-control diagnostic analysis involving plasma samples from psychiatric patients and control individuals collected between July 17, 2009 and May 18, 2018. Study participants were recruited as consecutive samples and volunteers in multiple inpatient and outpatient mental health hospitals in Western Europe (Germany and Austria [DE-AT]), China (CN), and Russia (UK).
This was a multi-cohort case-control diagnostic analysis involving plasma samples from psychiatric patients and control individuals collected between July 17, 2009 and May 18, 2018. Study participants were recruited as consecutive samples and volunteers at multiple inpatient and outpatient mental health hospitals in Europe (Germany and Austria [DE-AT]), China (CN), and Russia (UK). Samples and data were analyzed from January 2018 to September 2020.
Main results and measures
Plasma lipidome composition was assessed by liquid chromatography coupled with untargeted mass spectrometry.
Results
Blood lipid levels were assessed in 980 individuals (mean [SD] age, 36 [SD] years; 510 men [52%]) diagnosed with SCZ, BPD, MDD, or those with a first psychotic episode and in 572 controls ( mean age [SD], 34 [13] years; 323 male individuals [56%]).
A total of 77 lipids were found to be significantly altered between those with SCZ (n = 436) and controls (n = 478) in the 3 sample cohorts. Alterations were consistent between cohorts (CN and RU: [Pearson correlation] r = 0.75; DE-AT and CN: r = 0.78; DE-AT and RU: r = 0.82; P < 10 −38).
A lipid-based predictive model separated SCZ patients from controls with high diagnostic ability (area under the receiver operating characteristic curve = 0.86-0.95).
Lipidome alterations in BPD and MDD, evaluated in 184 and 256 individuals, respectively, were found to be similar to those in SCZ (BPD: r = 0.89; MDD: r = 0.92; P < 10 −79).
Evaluation of the alterations detected in individuals with a first psychotic episode, as well as in SCZ patients not receiving medication, demonstrated only a limited association with medication restricted to particular lipids.
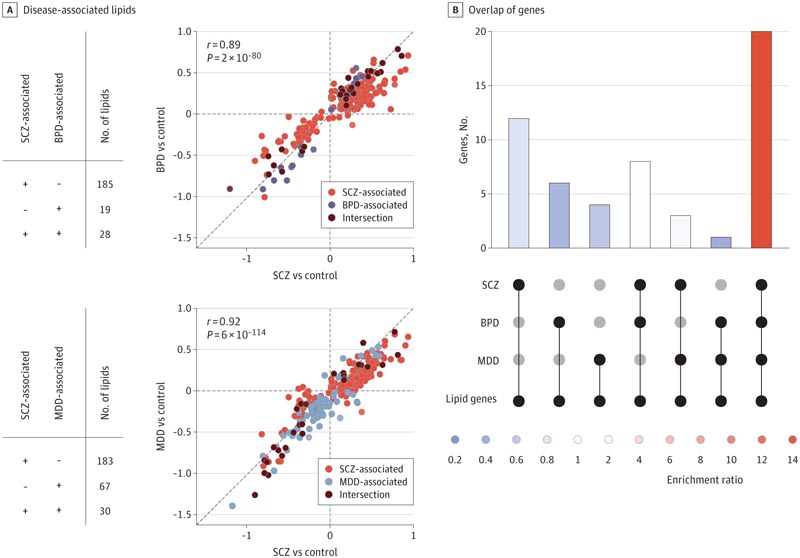
Figure: Comparison of blood plasma lipidome alterations between 3 psychiatric disorders. A, Number of disease-associated lipids that are common (+ +) or different (− +, + −) for the disorders and pairwise comparisons of log ratios of average lipid abundance (log2 fold change) between the different disorders and controls. Log2 changes were averaged for 3 (for schizophrenia [SCZ]) or 2 (for bipolar disorder [BPD] and major depressive disorder [MDD]) cohorts. The circles represent the lipid characteristics associated with SCZ, BPD and MDD, as well as their intersection. The diagonal line indicates y = x. B, Intersection of genes associated with SCZ, BPD and MDD, considering only the subset of 84 genes related to blood plasma lipid level variation. Colors correspond to the fold enrichment, calculated for each group by subsampling random groups of genes of the same size 1000 times .
Conclusions and relevance
In this study, SCZ was accompanied by a reproducible profile of plasma lipidome alterations, not associated with symptom severity, medication, and demographic and environmental variables, and largely shared with BPD and MDD.
This lipid alteration signature may represent a trait marker of severe psychiatric disorders, indicating its potential to be transformed into a clinically applicable testing procedure.
Discussion
By taking advantage of the multi-cohort design of this diagnostic study, we searched for reproducible lipid alterations in the blood plasma of patients with SCZ and sought to evaluate their specificity with respect to MDD and BPD, paving the way toward a clinically applicable lipid-based test for psychiatric diagnosis. disorders We identified a set of 77 lipids significantly and reproducibly associated with SCZ in the 3 culturally and demographically diverse cohorts.
Furthermore, we demonstrated that a multivariate model based on annotated lipid subsets separated SCZ from control individuals with a predictive performance (AUROC) greater than 0.9. The model’s performance did not decrease when applied to an independent first-episode psychotic cohort, demonstrating its good generalization. Furthermore, the model demonstrated an AUROC greater than 0.9 using 20 to approximately 150 lipids as input, allowing flexible feature selection for future clinical applications.
Our investigation of MDD and BPD, performed in parallel with SCZ measurements, revealed substantial similarities of lipid alterations between the 3 disorders . This result aligns with the similarities of lipid alteration between disorders reported for particular lipid classes and individual disorders. Furthermore, the SCZ-associated alterations identified in our study were positively and significantly correlated with the lipid alterations reported not only for SCZ but also for patients with MDD and BPD.
In addition to similarities in lipidome effect, the 3 disorders show a well-established overlap of clinical manifestations and underlying genetic factors. Our reanalysis of SCZ, MDD, and BPD genomic associations reproduced this overlap and revealed significant enrichment of enzymes corresponding to lipid classes associated with the disorder, in line with recent findings. Furthermore, genes associated with plasma lipidome variation strongly overlapped with genetic markers shared by SCZ, MDD and BPD, suggesting a link between common aspects of the disorders in both genetics and lipid phenotypes.
Conclusions In this blood plasma lipidome diagnostic analysis performed in 3 independent cohorts of SCZ patients, the results suggest significant and reproducible abundance alterations of 77 lipids. Further analysis suggested that these alterations are present in individuals with first-episode psychosis , not associated with medication and symptom severity, and largely shared by patients with MDD and BPD. Consequently, we demonstrated that predictive models using between 20 and 150 of the lipids tested reliably separated people with SCZ and controls, laying the foundation for the development of lipid-based clinical assessment of the risks of psychiatric disorders. |