Symptomatic uncomplicated urinary tract infections ( uUTI) are one of the most common infections in the United States (US). They are defined by the presence of dysuria, frequency, urgency, and suprapubic pain in women without fever and functional abnormalities or anatomical findings of the urinary tract, without recent urinary instrumentation . Urinary tract infections (UTIs) account for a substantial proportion of antibiotics prescribed in primary care and account for 10.5 million outpatient care visits due to UTI or cystitis in the US, or 0.9% of all outpatient care visits.
Most UTIs are caused by Escherichia coli (E. coli) and the standard of care for UTIs are empiric oral antimicrobial agents with activity against certain gram-positive and gram-negative bacteria, including: fosfomycin, nitrofurantoin, trimethoprim-sulfamethoxazole, and β-lactams (amoxicillin-clavulanate, cefdinir, cefaclor, cefpodoxime-proxetil and cephalexin) as alternative agents in patients with allergies/intolerance to the first line. However, there is increasing antimicrobial resistance among E. coli, which is a global problem.
UTIs are common infections that occur in about 1 in 3 women by the age of 24, or 50 to 60% of all women over their lifetime. UTIs have a substantial effect on quality of life and represent a considerable burden on health care. For example, in a population survey conducted in England in 2014, Butler et al. found that 15% of patients reported that UTIs affected their daily life “a lot ,” 37% reported that it affected their daily life “quite a bit,” and 95% reported contacting a healthcare professional about their UTI most recent. Additionally, Ellis and Verma found that quality of life scores (based on the Short-Form 36 questionnaire) were lower across all assessment domains for American women with outpatient UTI compared with healthy controls. Evaluation and treatment of UTI costs several billion dollars annually worldwide and approximately $2 billion annually in the US.
While the effects of UTI on quality of life have been previously investigated, contemporary studies on the key drivers of health-related quality of life (HRQoL), loss of work productivity, use of healthcare resources , direct and indirect costs, activity deficiency and lack of satisfaction with treatment. Furthermore, previous studies on UTI have not made a clear distinction between complicated UTI and UNcomplicated UTI . Therefore, to better understand these factors, we conducted a survey examining patient-reported activity impairment, HRQoL, workplace productivity, health care resource use (HRU) related to uUTI. and costs in US women with a self-reported UTI in the past 60 days that was treated with an oral antibiotic.
Background
Uncomplicated urinary tract infections (uUTIs) are among the most common infections in the U.S. However, only a few studies describe the impact of uUTIs from the patient’s perspective.
Methods
A cross-sectional online survey of US women aged ≥18 years was conducted to assess the burden of UTI in relation to activity impairment, health-related quality of life (HRQoL), workplace productivity , healthcare resource use (HRU), and costs. Participants who self-reported an uUI in the previous 60 days treated with ≥1 oral antibiotic were included. Activity impairment was assessed with the Activity Impairment Assessment scale . Health-related quality of life ( HRQOL) was assessed using a modified short form 36 (SF-36). Direct costs were the sum of out-of-pocket and monetized HRU expenses; Indirect costs were calculated using Work Productivity and Activity Impairment (WPAI).
Participants were stratified by uUI recurrence, number of antibiotics prescribed for recent UTI, and treatment appropriateness (1 first-line/1 second-line/multiple antibiotics). Multivariable regression analysis assessed the relationship between stratifications and outcomes while controlling for demographic/clinical characteristics. Propensity score matching was used to compare participants to a matched population from the 2020 National Health and Welfare Survey (NHWS), to control for any impact of COVID-19 on responses.
Results
Among 375 participants , impaired activities included sexual intercourse (66.9%), sleep (60.8%), and exercise (52.3%). HRQOL was worse (p<0.0001) than the NHWS population (46.4 vs. 51.3 [physical component score]; 40.0 vs. 46.9 [mental component score]; 0.63 vs. 0.72 [health utility index]).
All included WPAI assessments were worse for the uUTI vs. NHWS cohort (p<0.0001).
Adjusted direct costs were higher for participants receiving 2 vs. 1 antibiotic ($2090 vs. $776; p<0.0001) and receiving multiple vs. 1 first-line antibiotics ($1642 vs. $875; p=0.002) .
Recurrent UTI was associated with greater activity impairment , worse HRQOL, and costs compared with nonrecurrent.
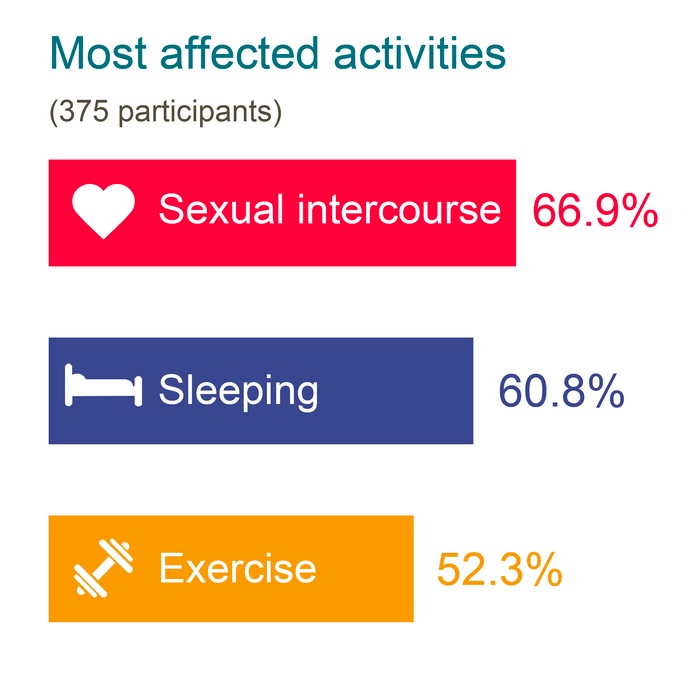
The graph shows the activities reported by survey participants as most affected by their recent uncomplicated urinary tract infection.
Conclusions
UTIs were associated with greater activity impairment, worse productivity, and reduced HRQoL. Higher costs were found versus a matched population.
Discussion
Urinary tract infections affect the sex life, sleep and exercise of more than half of women who experience them, and are associated with reduced quality of life, according to a US survey.
Among women, UTIs are a common occurrence. In our recall-based study, 43% of women had recurrent urinary tract infections, which was higher than the prevalence reported in the literature, which ranged from 20% to 40%. Despite this prevalence, the burden of the disease in patients is not well understood. We found that HRQoL scores, particularly MCS, were worse among participants with uUTI than a matched population based on the NHWS 2020. Similarly, WPAI measures were significantly affected by uUTI compared to the NHWS cohort. These data demonstrate the substantial burden that UITU represents for patients.
Additionally, we found that survey participants with recurrent uUTIs (43.5%) showed a higher level of activity impairment (shopping, housework/chores, and socializing, and the impact of WPAI on daily activities), worse HRQoL. (PCS, SF-6D) and productivity scores (presenteeism, general work impairment), higher mean total out-of-pocket costs, and higher mean total indirect costs compared to participants with nonrecurrent UTI.
The burden of recurrent UTIs from the patient’s perspective was previously described in a qualitative study of comments in an online forum that demonstrated the substantial and varied impact that repeat infections have on people’s quality of life. As with our study, these authors found that sexual intercourse is a commonly affected activity. Additionally, an online survey of women with recurrent UTIs in 5 European countries found that between 23% and 55% of participants (depending on the country and whether participants had a current acute UTI or had had one in the last 4 weeks) had physical health scores below a comparator of the general US population, and between 55% and 81% had mental health scores below the comparator. This is consistent with our study where a greater proportion of the cohort had MCS scores below the general population than PCS scores. However, our study has the strength of providing a comparison between recurrent and non-recurrent UTIs, allowing us to demonstrate the additional HRQoL burden that patients with recurrent UTIs have beyond that conferred by the infection alone.
When stratified by the number of oral antibiotics used, participants who received ≥3 antibiotics for their most recent uUI reported worse HRQoL (PCS, SF-6D) than those who received only 1 antibiotic. This could be because these participants have more severe disease or receive inappropriate treatment, resulting in more prescriptions, resulting in greater patient burden. However, our methodology excluded participants with more severe UTI and asymptomatic bacteriuria, resulting in a population with symptomatic UTI. Although we did not exclude participants with concurrent infections, the survey questions related specifically to their uUI.
Similarly, when stratified by use of clinically appropriate oral antibiotics, participants receiving multiple antibiotics had worse HRQoL (PCS, SF-6D) and a higher level of activity impairment (impact of WPAI on daily activities ) than those who received 1 appropriate antibiotic and a higher mean total direct cost than those who received 1 inappropriate antibiotic.
Regarding treatment satisfaction , participants with recurrent UTIs who received more than one antibiotic were found to be less satisfied with treatment than those with nonrecurrent UTIs successfully treated with one antibiotic. These data paralleled other endpoints, i.e., recurrent UTI and more antibiotics were associated with worse outcomes. High levels of satisfaction associated with single antibiotic therapy have previously been reported.
The increased direct costs related to uUI that we observed with the use of multiple versus single oral antibiotics could be due to inefficient prescribing. Inappropriate antibiotic prescribing based on drug class and duration of therapy has previously been shown to be prevalent in the treatment of UTI. Our results, however, suggest that ineffective therapies are prescribed as patients require multiple antibiotics to resolve their UTIs. Therefore, identifying the most appropriate antibiotic therapy may help optimize the direct UTI-related costs associated with antibiotic treatment. The use of multiple antibiotics may also increase the risk of developing antimicrobial resistance , which is a growing problem globally, and is not consistent with antibiotic stewardship practices. E. coli , the predominant uropathogen responsible for UTI, is a common causative pathogen of other diseases and a World Health Organization priority pathogen, identified as being at critical risk for antimicrobial resistance.
The most common healthcare resource used by participants to treat their recent UTI was visits to their primary care physician followed by urgent care visits and visits to their OB/GYN . The majority of total direct costs were due to PCP visits and urgent care visits. Compared to the general population, uUTI had a significant impact on absenteeism and presenteeism , resulting in indirect costs that most directly affect employers, specifically those that provide health insurance to employees (70% of the sample paired). Insurers that provide coverage to employers and employers that contract with insurers for employer-sponsored health care plans must account for the indirect costs related to UUI episodes in addition to the direct costs of treatment.
Consistent with our study, a multi-country observational study found that anxiety and depression were the most commonly reported comorbidities among women with uUI at baseline. Furthermore, the HRQoL scores (PCS and MCS) reported in our study were similar to those reported in a French study of patients with cystitis or other female genital diseases; with a mean PCS of 45.6 and MCS of 41.5 compared to 46.5 and 40.0 in the current study, respectively.
Final message This study demonstrates that uUIs are significantly associated with worse patient-reported outcomes, such as daily activities, work productivity, and mental HRQoL, and that suboptimal treatment (i.e., use of multiple antibiotics) may play a role. Inadequate response to treatment, evident by the use of multiple antibiotics to treat a UTI, was associated with an increase in UTI-related costs, including loss of productivity. While UTIs are common, their impact on patients should not be underestimated; Appropriate treatment is crucial to prevent adverse impacts on quality of life and healthcare resources (HRU). |
















