
Prostatic artery embolization ( PAE) provides long-term effectiveness in treating urinary symptoms of an enlarged prostate gland, according to new research to be presented at the Society of Radiology Annual Scientific Meeting Interventionist in Phoenix.
Purpose: PAE is a minimally invasive treatment of lower urinary tract symptoms (LUTS) and urinary retention secondary to BPH. This study evaluates and expands the efficacy and safety profile of PAE in the treatment of BPH with LUTS or urinary retention. Materials and methods: A total of 1,000 patients underwent PAE for BPH with LUTS or urinary retention from January 2014 to September 2022. The mean age of the patients was 70.2 ± 9.5 years, the mean prostate volume was 107.2 ± 65.1 g, the median IPSS and QoL scores before the procedure were 23 (IQR, 18 -28) and 5 (IQR, 4-6), respectively. Transradia l access was performed in 820 procedures. Patient evaluation was carried out at intervals of 6-12, 24, 60 and 72 months (mo) after PAE. Adverse events were recorded using the Clavien-Dindo (CD) classification. A two-tailed P < 0.05 was considered significant. Results: Median follow-up was 1027 days (range, 39-3184). Follow-up data for 3-12, 24, 60, and 72 months are reported in the table. 6-12 months after PAE, median IPSS decreased to 6 (IQR 3-10) (n ¼ 615; P < 0.01), median quality of life was 1 (IQR 0-2) ( n ¼ 615; P < 0.01) and the mean prostate size was 70.9 ± 44.7 g (n = 175; P < 0.01). 24 months after PAE, median IPSS was 7 (IQR 3-14) (n ¼ 106; P < 0.01), median QoL was 1 (IQR 0-3) (n ¼ 106 P < 0.01) and the mean prostate size was 82.9 ± 47.1 g (n = 59; P < 0.01). 5 years after PAE, median IPSS was 3 (IQR 2-14) (n ¼ 35 P < 0.01), median QoL was 1 (IQR 0-2) (n ¼ 35 P < 0.01 ) and the mean prostate size was 69.3 ± 23.3 g (n = 7; P < 0.01). 6 years after PAE, median IPSS was 6 (IQR 3-11) (n ¼ 10 P < 0.01) and median QoL was 0.5 (IQR 0-1.8) ( n ¼ 10 P < 0.01). 67 patients (6.7%) have required a second procedure for recurrent LUTS; 10 underwent a second PAE. Self-limited postoperative symptoms of frequency, urgency, and dysuria (CD grade I) occurred in 33.5% of patients. 3 patients had non-target embolization with penile ulceration (CD grade II) that resolved with local conservative measures. 3 patients (0.3%) developed urosepsis (CD grade IV) and were treated with IV antibiotics. 3 patients had TIAs that resolved without further intervention. Conclusion: PAE is an established safe and clinically effective procedure for patients with LUTS secondary to BPH with excellent short- and medium-term results. Long-term results, including sustained relief of LUTS and significant improvement in QoL, remain promising. |
Comments
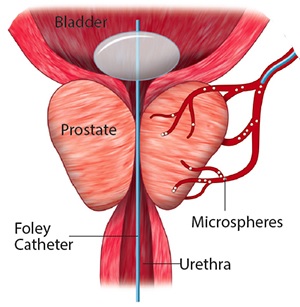
In the largest long-term study in North America, 1,000 patients undergoing PAE reported significant sustained relief, for up to six years , of lower urinary tract symptoms (LUTS) or urinary retention due to benign prostatic hyperplasia (BPH ). HPB). BPH is the most common benign condition in men, affecting more than 50% of men over 60 years of age. The prostate gland enlarges with age, putting pressure on the urethra, which carries urine from the bladder, often causing urinary urgency, increased frequency and inconsistency of flow, straining to urinate, and inability to completely empty the bladder.
“Our study shows that PAE is a highly effective treatment whose long-term results include sustained relief of LUTS and significant improvement in quality of life,” said senior author Shivank Bhatia, MD, Chair of Interventional Radiology at the University of Miami Miller School of Medicine. “Of the 18 million men in the U.S. eligible for BPH treatment, many avoid all treatments due to the widely known risks of surgery, particularly sexual side effects and leaks. “PAE avoids these risks while achieving positive long-term clinical outcomes.”
With PAE, interventional radiologists inject tiny particles into the arteries that feed the prostate gland, reducing its blood supply and therefore shrinking it. Researchers say PAE shows "excellent short- and medium-term results" and positive long-term results in improving self-reported symptoms.
Participants reported dramatic improvements on the 35-point International Prostate Symptom Score , which classifies symptoms as mild, moderate or severe. Before the procedure, patients reported a mean score of 23, in the "severe" range . But in less than three months, they achieved a score of 6, with "mild" symptoms that persisted throughout the six-year study , a response similar to that which followed more invasive surgical options for BPH. However, PAE did not have a negative impact on sexual function and no incidence of leakage was reported after PAE.
Study participants were also asked a quality of life question: "If you had to spend the rest of your life with your urinary condition the way it is now, how would you feel about it?" Before the procedure, the average score was 5, or "mostly dissatisfied ," but within a year, the score was 1, or "mostly satisfied ," a rating that also continued throughout the process.
PAE has a well-established safety profile , as shown in repeated studies in the 10 years since it was first used. However, interventional radiologists say most men are unaware of this treatment option. Most will avoid surgery and instead may take medications for years, even as BPH worsens, which can lead to bladder failure.
"Patients choose ECPs to avoid the side effects of current BPH medications, which may include erectile dysfunction, painful or difficult urination, constipation, dizziness, or fatigue," said study lead author Andrew Richardson, MD, senior resident. from Jackson Memorial Hospital in Miami. “Prostatic artery embolization is an alternative not only to surgery, but also to lifelong medication . ”
Among the study’s findings was a persistent reduction in prostate size for years. However, Bhatia noted that reducing prostate size is not the only goal in long-term effectiveness. “Treatment should make the prostate softer and smaller, rather than making it smaller but remaining hard, which will still cause urinary symptoms.”
Bhatia, the lead operator (or treating doctor) for all patients in the study, encourages patients to learn about all the options for their enlarged prostate symptoms, talk to several doctors, and then decide what is best for them. Bhatia says, "One size does not fit all when it comes to treating BPH, and PAE remains a very attractive alternative for patients with larger glands and in situations of acute urinary retention."
Abstract #3: Prostate Artery Embolization - Single Center Experience of 1000 Patients with Short, Mid, and Long Term Follow Up. A. Richardson, A. Maini, K. Richardson, K. Shah, A. Bhatia, R. Reddy, A Sanan, J. Kumar, H. Jalaeian, S. Bhatia. Annual Scientific Meeting, March 4–9, 2023.















