Spinal cord stimulation, a medical technology suggested to treat people with chronic back pain, does not provide long-term relief and may cause harm, according to a Cochrane review .
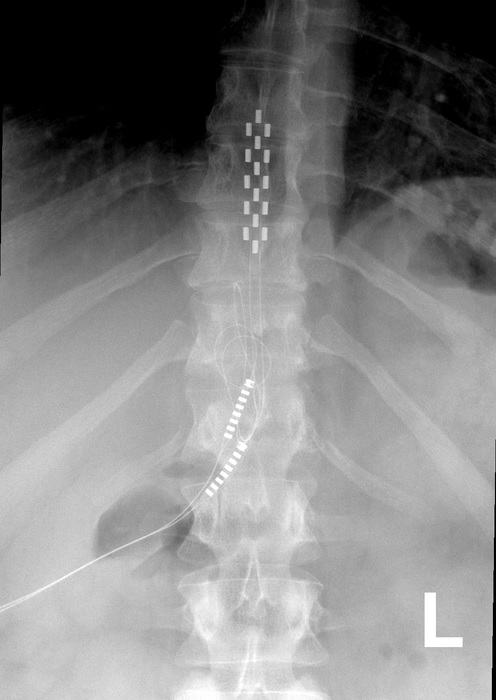
X-ray of a human spine with spinal cord stimulator implant. Credit. Mconnell, CC BY 3.0 , via Wikimedia Commons https://commons.wikimedia.org/wiki/File:Anterior_thoracic_SCS.jpg
Spinal cord stimulation is thought to work by implanting a device that sends electrical pulses to the spinal cord to interrupt nerve signals before they reach the brain.
The study reviewed published clinical data on spinal cord stimulation. This included randomized controlled trials, considered the most robust method of measuring the effectiveness of a treatment in medical research.
Researchers analyzed the results of 13 clinical trials, looking at data from 699 participants, and compared spinal cord stimulation treatment with placebo or no treatment for low back pain.
Researchers, medical professionals, and policymakers rely on Cochrane reviews because they use robust methodologies to combine evidence from multiple sources, reducing the impact of bias and random error that can make individual studies less reliable.
The review concluded that spinal cord stimulation is no better than a placebo for treating low back pain, with probably little or no benefit for people with low back pain or an improvement in their quality of life. There was little or no clinical data regarding the long-term effectiveness of spinal cord stimulation.
The researchers also found that the adverse side effects of surgery were generally poorly documented, preventing them from concluding the level of risk involved. Damage from spinal cord stimulation can include nerve damage, infection, and movement of electrical wires, all of which may require repeat surgeries.
The results of the review have been sent to the Federal Department of Health and Aged Care’s prosthetic list review working group. The task force is reviewing the eligibility of current Medicare-subsidized prosthetics.
In Australia, the safety and long-term performance of the devices is also being re-evaluated by The Therapeutic Goods Administration (TGA), the country’s regulatory authority for therapeutic products.
“Spinal cord stimulation is invasive and has a large financial cost for people who choose surgery as a last resort to relieve their pain. “Our review found that the long-term benefits and harms are essentially unknown,” said lead researcher Dr Adrian Traeger of Sydney Musculoskeletal Health , an initiative of the University of Sydney, the Sydney Local Health District and the District of North Sydney Local Health.
"Our review of the clinical data suggests that no sustained benefit from surgery outweighs the costs and risks."
“Low back pain is one of the leading causes of disability worldwide. Our findings further emphasize the urgent need to review funding arrangements for chronic pain care to assist patients in their search for relief. There are evidence-based physical and psychological therapies for back pain; Guaranteeing access to these is essential.”
The review team found multiple gaps in the clinical data. There were no studies investigating the long-term impact (more than 12 months) of spinal cord stimulation on low back pain. The longest was a single six-month trial. Most clinical trials only looked at the immediate impact of the device, which is a time frame of less than a month.
The review team provided a list of recommendations, including that future spinal cord stimulation clinical trials last at least 12 months, clearly document the number of people experiencing adverse events, and make comparisons with other pain treatment options.
Professor Chris Maher, co-director of Sydney Musculoskeletal Health, said: “Our review found that the clinical benefit of adding spinal cord stimulation to treat low back pain is still unknown. When combined with the reality that these devices are very expensive and often break, there is clearly an issue here that should concern regulators.”
A separate Cochrane review, in which the researchers were not involved, examined the effect of spinal cord stimulation versus placebo in people with chronic pain. Similar to this review, it concluded that there was a lack of evidence to suggest long-term benefits in the treatment of chronic pain.
Authors’ conclusions The data in this review do not support the use of spinal cord stimulation (SCS) to manage low back pain outside of a clinical trial. Current evidence suggests that SCS is unlikely to have sustained clinical benefits that outweigh the costs and risks of this surgical intervention. |















