Key points: - The study analyzes the association between COVID-19 and gastrointestinal diseases. - Data from two cohorts of patients with and without COVID-19 were used. - Variables that occurred in at least 100 participants in each exposure group were selected. - The univariate relative risks between each variable and the exposure were estimated. - 100 variables with the highest relative risks were selected for use in statistical analyses. - COVID-19 patients are at increased risk of developing gastrointestinal diseases compared to historical and contemporary controls. - Diarrhea is the most common gastrointestinal symptom in patients with COVID-19. - The presence of gastrointestinal diseases is associated with an increased risk of hospitalization and death in patients with COVID-19. - More studies are needed to better understand the relationship between COVID-19 and gastrointestinal diseases. |
Summary:
The study examines the relationship between COVID-19 and gastrointestinal diseases using data from two patient cohorts. Variables that occurred in at least 100 participants in each exposure group were selected, and univariate relative risks between each variable and the exposure were estimated. The 100 variables with the highest relative risks were used for statistical analyses.
The conclusions of the article indicate that patients with COVID-19 have an increased risk of developing gastrointestinal diseases, especially diarrhea. Additionally, the presence of gastrointestinal diseases is associated with an increased risk of hospitalization and death in patients with COVID-19. However, more studies are needed to better understand the relationship between COVID-19 and gastrointestinal diseases.
SARS-CoV-2 infection can cause a wide range of post-acute sequelae that can affect pulmonary and extrapulmonary organs, including the gastrointestinal system; The constellation of these post-acute conditions is known by the general term long COVID . Studies investigating post-acute gastrointestinal sequelae of SARS-CoV-2 infection are mainly limited to hospitalized people and all had a short follow-up duration of a few months, and a limited selection of outcomes. A comprehensive assessment of the risks and burdens of gastrointestinal disorders in the post-acute phase of COVID-19 is needed but has not yet been performed. Addressing this knowledge gap is important to inform post-acute COVID-19 care strategies.
In this work, we used the US Department of Veterans Affairs national healthcare databases to create a cohort of 154,068 people who survived the first 30 days of COVID-19 and two control groups including a contemporary control of 5,638,795 who lived during the same time but had no evidence of SARS-CoV-2 infection, and a historical cohort of 5,859,621 people from the pre-pandemic era. These cohorts were followed longitudinally to estimate the 1-year risks and burdens of a set of prespecified incident gastrointestinal outcomes in the overall cohort and by care setting of the acute phase of SARS-CoV-2 infection (i.e., whether people were not -hospitalized, hospitalized or admitted to intensive care).
A comprehensive assessment of the 1-year risks and burdens of gastrointestinal disorders in the post-acute phase of COVID-19 is needed but not yet available.
We show that beyond the first 30 days of infection, people with COVID-19 exhibited increased 1-year risks and burdens of incident gastrointestinal disorders spanning several disease categories, including motility disorders, acid-related disorders (dyspepsia , gastroesophageal reflux disease, peptic ulcer disease), functional intestinal disorders, acute pancreatitis, liver and biliary disease .
Risks were evident in people who were not hospitalized during the acute phase of COVID-19 and increased gradually across the severity spectrum of the acute phase of COVID-19 (non-hospitalized, hospitalized, and admitted to intensive care ).
Risks were consistent in comparisons that included COVID-19 versus contemporary control group and COVID-19 versus historical control group as the reference category.
Figure: 1-year risks and burdens of incident COVID-19 post-acute composite gastrointestinal outcomes compared to contemporary control cohort.
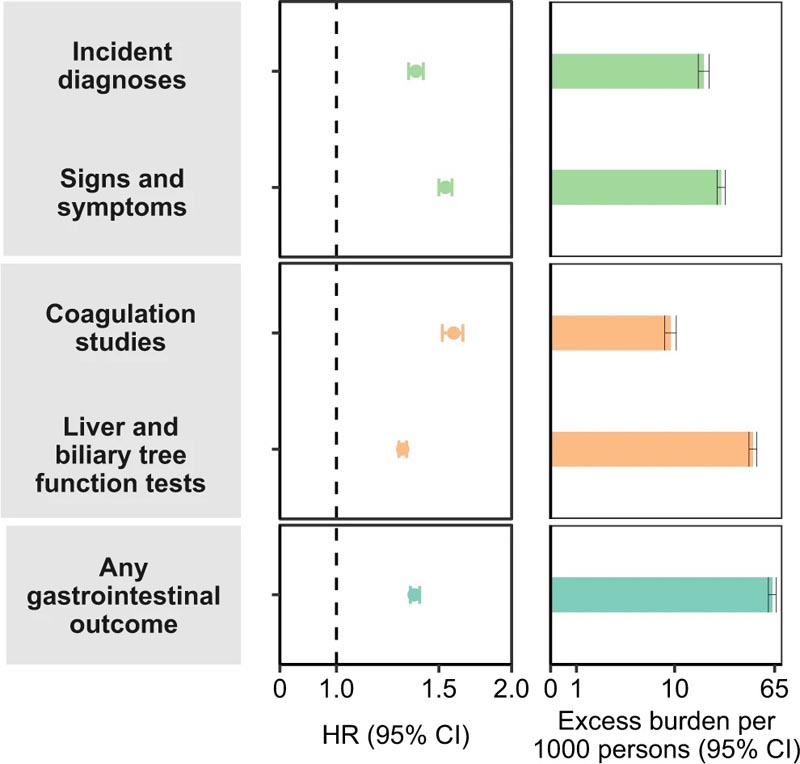
Composite outcomes consisted of incident diagnoses (GERD, PUD, acute pancreatitis, functional dyspepsia, acute gastritis, IBS, and cholangitis), signs and symptoms (constipation, abdominal pain, diarrhea, vomiting, and bloating), coagulation studies (PT, PTT, INR), liver and biliary tree function tests (albumin, ALT, total protein, AST, LDH, CRP, ALP, total bilirubin, GGT, direct bilirubin, lipase and amylase) and any gastrointestinal findings (incident occurrence of any gastrointestinal findings studied ). Results were determined 30 days after positive COVID-19 test until the end of follow-up. COVID-19 cohort (n=154,068) and contemporary control cohort (n=5,638,795). Adjusted HRs (dots) and 95% CIs (confidence intervals) (error bars) are presented, as are estimated excess burdens (bars) and 95% CIs (error bars). The burdens are presented per 1000 people at 12 months of follow-up. The dashed line marks a HR of 1.00; lower limits of the 95% CIs with values greater than 1.00 indicate a significantly increased risk. GERD gastroesophageal reflux disorder, IBS irritable bowel syndrome, PT prothrombin time, PTT partial thromboplastin time, INR international normalized ratio, ALT alanine transaminase, AST aspartate transaminase, LDH lactate dehydrogenase, CRP c-reactive peptide, ALP alkaline phosphatase, GGT γ-glutamyl transferase.
Taken together, our results show that people with SARS-CoV-2 infection are at increased risk of gastrointestinal disorders in the post-acute phase of COVID-19. Post-COVID care should include attention to gastrointestinal health and disease.
Discussion
In this work involving 11,652,484 people, including 154,068 people with COVID-19, 5,638,795 contemporary controls and 5,859,621 historical controls, which in total correspond to 14,064,985 people per year of follow-up, we provide evidence that more Beyond the first 30 days of infection, people with COVID-19 19 exhibited increased risks and 1-year burdens of incident gastrointestinal disorders spanning several disease categories, including motility disorders, acid-related disorders (dyspepsia, GERD , PUD), functional intestinal disorders, acute pancreatitis, liver and biliary disease.
Risks were evident in subgroups based on age, race, sex, obesity, smoking, cardiovascular disease, chronic kidney disease, diabetes, hyperlipidemia, and hypertension. Risks were evident in people who were not hospitalized during the acute phase of COVID-19 and increased gradually across the spectrum of severity of the acute phase of COVID-19 (from non-hospitalized people to hospitalized people, to those who were admitted to intensive care). Risks were consistent in comparisons that included COVID-19 versus contemporary control group and COVID-19 versus historical control group as the reference category.
A comparative analysis suggested that people hospitalized with COVID-19 are at increased risk for several gastrointestinal outcomes compared to people hospitalized with seasonal influenza. Results were consistently robust to challenge in several sensitivity analyses; and examination of a positive outcome control, a battery of negative outcome controls, and a pair of exposure controls yielded results consistent with pretest expectations. The constellation of findings suggests that people with SARS-CoV-2 infection are at increased risk of gastrointestinal disorders in the post-acute phase of COVID-19. The risks and burdens are not trivial, suggesting that acute post-Covid care strategies should include attention to gastrointestinal disease.
Our findings suggest that gastrointestinal disease is another facet of the multifaceted long COVID.
The risks were evident even in people whose acute illness did not require hospitalization. This group represents the majority of people with COVID-19. Although the absolute burdens (expressed per 1000 people in 1 year) may seem small, due to the large number of people with SARS-CoV-2 infection, these rates may translate into a large number of affected people. This will have ramifications not only for the personal health of those affected, but also for the health systems that will need to address the care needs of people with post-acute gastrointestinal disorders due to COVID-19.
In summary , in this study of 154,068 people who survived the acute phase of COVID-19, we show an increased risk and burden of post-acute gastrointestinal sequelae spanning several disease categories, including acidic disorders, functional intestinal disorders, pancreatic disorders, liver and biliary diseases. The risks were evident even among those whose acute COVID-19 did not require hospitalization. Our findings suggest that post-acute COVID-19 care strategies should include attention to gastrointestinal health and disease.