Summary Justification : Obesity affects 40% of American adults, is associated with a pro-inflammatory state, and presents a significant risk factor for the development of severe coronavirus disease (COVID-19). To date, there is limited information on how obesity might affect immune cell responses in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Goals : Ddetermine the impact of obesity on respiratory tract immunity in COVID-19 across the human lifespan. Methods: We analyzed single-cell transcriptomes of BAL in three cohorts of ventilated adults with (n = 24) or without (n = 9) COVID-19 from nasal immune cells in children with (n = 14) or without (n = 19) COVID-19, and peripheral blood mononuclear cells in an independent cohort of adults with COVID-19 (n = 42), comparing obese and non-obese subjects. Measurements and main results: Surprisingly, we found that obese adult subjects had attenuated pulmonary immune or inflammatory responses in SARS-CoV-2 infection, with decreased expression of IFN-α, IFN-γ, and TNF-α (tumor necrosis factor α) gene signatures. of response in almost all subsets of lung immune and epithelial cells, and lower expression of IFNG and TNF in specific lung immune cells. Peripheral blood immune cells in an independent adult cohort showed a similar but less marked reduction in type I IFN and IFNγ response genes, as well as a decrease in serum IFNα, in obese patients with SARS-CoV-2. Nasal immune cells from obese children with COVID-19 also showed reduced enrichment of the IFN-α and IFN-γ response genes. Conclusions: These findings show attenuated tissue immune responses in obese patients with COVID-19, with implications for treatment stratification, supporting the targeted application of inhaled recombinant type I IFNs in this vulnerable subset. |
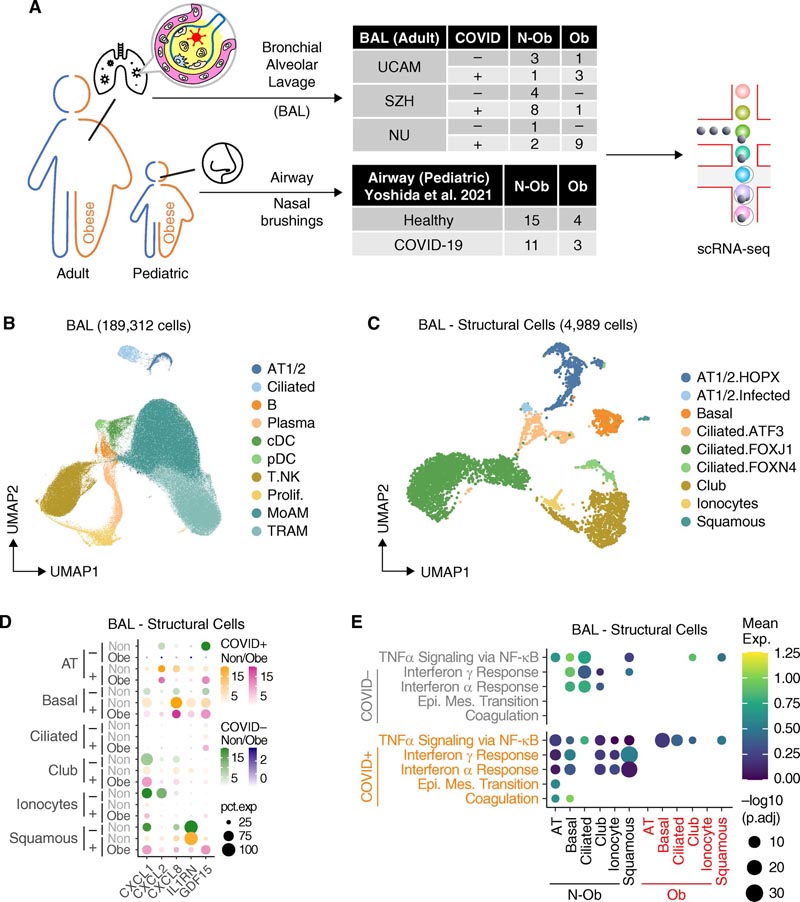
Single-cell analysis of BAL fluid samples from patients with or without coronavirus disease (COVID-19) reveals differences in gene set enrichment in structural cells in nonobese subjects compared to obese subjects. (A) Workflow overview. In this study, we included BAL samples from 33 patients from three cohorts with BMI information, namely, UCAM (University of Cambridge) (n = 8; ob = 3; this study), SZH (Shenzhen Third Hospital) (n = 13; ob = 1; Liao and colleagues [18]) and NU (Northwestern University) (n = 12; ob = 9; Grant and colleagues [19]). BMI data in pediatric subjects with airway sampling were obtained from Yoshida and colleagues (20). (B) Uniform manifold approximation and projection (UMAP) embedding of 189,312 cells after integration of the three data sets. Cells are colored according to the harmonized wide cell type annotations. (C) UMAP embedding of 4,989 epithelial and structural cells after integration colored according to harmonized fine cell type annotations. (D) Dot plot of mean expression of the main cytokines and chemokines differentially expressed in each epithelial subpopulation in COVID+ BAL samples. The amounts of expression in each case are indicated by different color gradients (green: non-obese without COVID-19; yellow: non-obese with COVID-19; purple: obese without COVID-19; and magenta: obese with COVID-19). . Expression percentages are indicated by dot size. Unidentified basal, ciliated, and club cells in obese individuals without COVID-19 samples are not shown. (E) Dot plot of mean expression of the five most enriched immune pathways within Hallmark gene sets for epithelial/structural cells. The mean expression of the genes contained in each gene set within each cell type, separated into non-obese vs. obese groups, are indicated by color gradients. P values are indicated by point sizes. AT = alveolar type; BMI = body mass index; Epi. Month. = epithelial mesenchyme; exp = expression; N-ob = not obese; ob = obese; pct.exp = expression percentage; prolific = proliferate; scRNAseq = single cell RNA sequencing.
Comments
Scientific knowledge on the subject
Obese people are known to be at higher risk of developing severe coronavirus disease (COVID-19), with the subsequent risks of needing mechanical ventilation and subsequent death. However, the mechanisms underlying these increased risks are not well described.
What this study adds to the field
This study identified attenuated immune responses in immune cells from the respiratory tract and peripheral blood of obese patients with COVID-19 compared to non-obese patients. Reduced type I and type 2 IFN responses were identified in all compartments and in multiple immune cell types in which reduced TNF-α (tumor necrosis factor α) signaling was identified in alveolar but not peripheral blood cells. These data provide important insights into the mechanisms of severe COVID-19 disease in obesity and suggest potential therapeutic approaches.
Obese people may be more susceptible to severe COVID-19 due to a poorer inflammatory immune response, Cambridge scientists say.
Scientists from the Cambridge Institute of Therapeutic Immunology and Infectious Diseases (CITIID) and the Wellcome Sanger Institute showed that after SARS-CoV-2 infection, cells in the lining of the lungs, nasal cells and immune cells in the blood show an attenuated inflammatory response in obese patients, producing suboptimal levels of molecules necessary to fight infection.
Since the start of the pandemic, there have been almost 760 million confirmed cases of SARS-CoV-2 infection, with almost 6.9 million deaths. While some people have very mild symptoms, or even no symptoms at all, others have much more severe symptoms, including acute respiratory distress syndrome that requires respiratory assistance.
One of the main risk factors for severe COVID-19 is obesity, defined as a body mass index (BMI) greater than 30. More than 40% of American adults and 28% of English adults are classified as obese.
While this link has been demonstrated in numerous epidemiological studies, until now it was unclear why obesity should increase a person’s risk of severe COVID-19. One possible explanation was thought to be that obesity is linked to inflammation: studies have shown that obese people already have higher levels of key molecules associated with inflammation in their blood. Could an overactive inflammatory response explain the connection?
Professor Menna Clatworthy is a clinical scientist at the University of Cambridge who studies tissue immune cells at CITIID and cares for patients at Addenbrooke’s Hospital, part of Cambridge University Hospitals NHS Foundation Trust. She said: “During the pandemic, most of the younger patients I saw on COVID wards were obese . Given what we know about obesity, if you had asked me why this was the case, I would have said it was most likely due to excessive inflammation. What we found was the complete opposite.”
Clatworthy and his team analyzed blood and lung samples taken from 13 obese patients with severe COVID-19 requiring mechanical ventilation and intensive care treatment, and 20 controls (nonobese COVID-19 patients and ventilated non-COVID-19 patients). These included patients admitted to the Intensive Care Unit at Addenbrooke’s Hospital.
His team used a technique known as transcriptomics, which analyzes the RNA molecules produced by our DNA, to study the activity of cells in these key tissues. Their results are published in the American Journal of Respiratory and Critical Care Medicine.
Contrary to expectations, the researchers found that obese patients had underactive immune and inflammatory responses in their lungs.
In particular, compared with non-obese patients, the cells in the lining of their lungs and some of their immune cells had lower levels of activity among the genes responsible for the production of two molecules known as interferons (INF): interferon-alpha and interferon. -gamma – which help control the response of the immune system, and tumor necrosis factor (TNF), which causes inflammation.
When they looked at immune cells in the blood of 42 adults from an independent cohort, they found a similar, but less marked, reduction in the activity of interferon-producing genes, as well as lower levels of IFN-alpha in the blood.
Professor Clatworthy said: “This was really surprising and unexpected. In all cell types we analyzed, we found that the genes responsible for the classical antiviral response were less active. “They were completely silenced.”
The team was able to replicate their findings in nasal immune cells taken from obese children with COVID-19, where they again found lower levels of activity between the genes that produce IFN-alpha and IFN-gamma. This is important because the nose is one of the entry points for the virus: a strong immune response there could prevent the infection from spreading further through the body, while a poorer response would be less effective.
One possible explanation for the finding involves leptin , a hormone produced in fat cells that controls appetite. Leptin also plays a role in the immune response: in people who are of normal weight, levels of the hormone increase in response to infection and it directly stimulates immune cells. But obese people already have chronically higher levels of leptin, and Clatworthy says they may no longer produce enough extra leptin in response to infection , or may be desensitized to it, leading to inadequate stimulation of their immune cells. .
The findings could have important implications for both the treatment of COVID-19 and the design of clinical trials to test new treatments.
Because an overactive immune and inflammatory response may be associated with severe COVID-19 in some patients, doctors have turned to anti-inflammatory medications to dampen this response. But anti-inflammatory medications may not be appropriate for obese patients.
Co-author Dr Andrew Conway Morris, from the Department of Medicine at the University of Cambridge and honorary consultant to the intensive care unit at Addenbrooke’s Hospital, said: "What we have shown is that not all patients are the same, so "We may need tailored treatments. Obese subjects may need fewer anti-inflammatory treatments and potentially more help for their immune system."
Clinical trials for potential new treatments would have to involve stratification of patients rather than including both severely ill and normal-weight patients, whose immune responses differ.
The research was largely supported by Wellcome, the Medical Research Council and the National Institute for Health Research, including through the NIHR Cambridge Biomedical Research Centre.
Reference
Guo, SA, Bowyer, GS, Ferdinand, JR, Maes, M & Tuong, ZK et al. Obesity associated with attenuated tissue immune cell responses in COVID-19. Am J Resp Critical Care Med; Mar 1, 2023; DOI: 10.1164/rccm.202204-0751OC