Key points What symptoms are present differently in people infected with SARS-CoV-2 6 months or more after infection compared to uninfected people, and what symptom-based criteria can be used to identify sequelae ? post-acute cases of SARS-CoV-2 infection (PASC)? Findings In this analysis of data from 9764 participants in the RECOVER adult cohort, a prospective longitudinal cohort study, 37 symptoms across multiple pathophysiological domains were identified as more frequently present in participants infected with SARS-CoV-2 at 6 months or more after infection compared to uninfected participants. A preliminary rule was derived to identify post-acute sequelae of SARS-CoV-2 infection cases (PASC) based on a composite symptom score. Meaning A framework to identify cases of post-acute sequelae of SARS-CoV-2 infection cases (PASC) based on symptoms is a first step in defining PASC as a new condition. These findings require iterative refinement that further incorporates clinical characteristics to arrive at actionable definitions of PASC. |
More than 658 million people worldwide have been infected with SARS-CoV-2. Post- acute sequelae of SARS-CoV-2 infection (PASC), also known as long COVID and defined as ongoing, recurrent, or new symptoms or conditions present 30 or more days after infection, are an important clinical and health problem. public health. The short- and long-term effects of post-acute sequelae of SARS-CoV-2 infection cases (PASC) have substantial impacts on health-related quality of life, income, and healthcare costs. Most existing PASC studies have focused on the frequency of individual symptoms and have generated widely divergent prevalence estimates due to their retrospective design and lack of an uninfected comparison group. Furthermore, defining PASC precisely is difficult because it is heterogeneous, composed of conditions with variable and potentially overlapping etiologies (e.g., organ injury, viral persistence, immune dysregulation, autoimmunity, and gut dysbiosis).
It is of great scientific and public health importance to better investigate the underlying mechanisms of post-acute sequelae of SARS-CoV-2 infection cases (PASC) and potential preventive and therapeutic interventions. This effort requires the collection of data on SARS-CoV-2 infected and uninfected individuals in a large prospective cohort study designed specifically to characterize PASC. Furthermore, the simultaneous consideration of multiple symptoms that persist over time and the application of appropriate analytical techniques are essential. Further consideration of changes in the frequency of PASC and its manifestations over the course of the COVID-19 pandemic is important, due to variable SARS-CoV-2 strains, new treatment and prevention strategies, and repeated infections.
This study is part of the National Institutes of Health’s Researching COVID to Improve Recovery (RECOVER) Initiative, which seeks to understand, treat, and prevent PASC (https://recovercovid.org/). In this first analysis of data from the RECOVER adult cohort, we outline criteria for identifying post-acute sequelae of SARS-CoV-2 infection cases (PASC) based on self-reported symptoms and describe several distinctive PASC subphenotypes . with various impacts on well-being and physical health. This study was enriched with self-referred participants to promote inclusive participation. Estimates were expected to be most precise in the subcohort of participants enrolled within 30 days of acute infection, for whom PASC-based selection bias would be minimal.
Unlike electronic health records and most existing cohort studies, data from this study captured self-reported symptoms specific to PASC based on standardized questionnaires developed with input from patient representatives. This report is a prospective, adequately powered PASC study based on participant-reported symptoms that included infected and uninfected individuals over the course of the pandemic. Notably, unlike previous reports, the paradigm presented here is not based on predefined clinical symptoms; instead, a definition of PASC is proposed as a new condition specific to SARS-CoV-2 infection.
Importance
SARS-CoV-2 infection is associated with persistent, recurrent, or new symptoms or other health effects that occur after an acute infection, called post-acute sequelae of SARS-CoV-2 infection (PASC), also known as Long COVID . Characterization of PASC requires analysis of data collected prospectively and consistently from diverse infected and uninfected individuals.
Aim
To develop a definition of the post-acute sequelae of SARS-CoV-2 infection cases (PASC) using self-reported symptoms and describe the frequencies of PASC in the cohorts, vaccination status, and number of infections.
Design, environment and participants
Prospective observational cohort study of adults with and without SARS-CoV-2 infection at 85 enrollment sites (hospitals, health centers, community organizations) located in 33 states plus Washington, DC and Puerto Rico. Participants who enrolled in the RECOVER adult cohort before April 10, 2023 completed a symptom survey 6 months or more after the onset of acute symptoms or the date of testing. Selection included population-based, voluntary, and convenience sampling.
Exposure
SARS-CoV-2 infection.
Main results and measures
Post-acute sequelae of SARS-CoV-2 infection cases (PASC) and 44 symptoms reported by participants (with severity thresholds).
Results
A total of 9,764 participants (89% infected with SARS-CoV-2; 71% female; 16% Hispanic/Latino; 15% non-Hispanic black; median age, 47 years [IQR, 35-60]) met criteria of selection. Adjusted odds ratios were 1.5 or greater (infected vs. uninfected participants) for 37 symptoms.
Symptoms that contributed to the PASC score included:
|
Among 2,231 participants who were first infected on or after December 1, 2021 and enrolled within 30 days of infection, 224 (10% [95% CI, 8.8%-11%]) gave positive in PASC at 6 months.
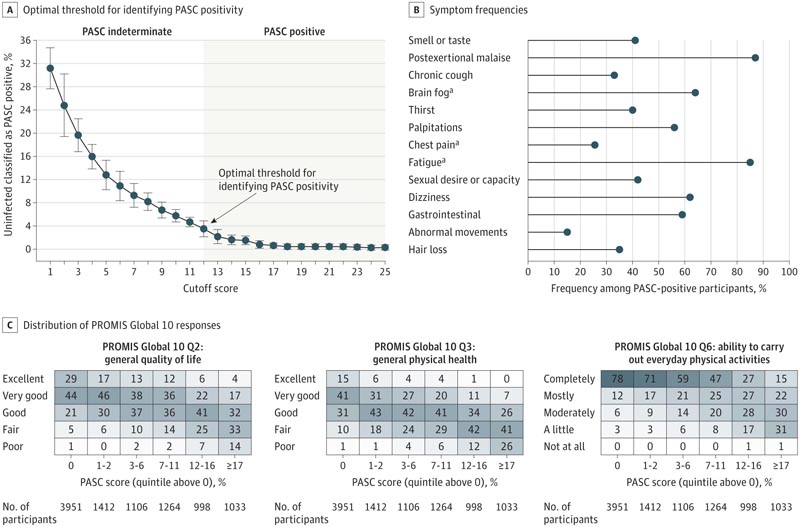
A, Optimal cutoff point for classifying a participant as PASC positive using cross-validation (eMethods in Supplement 3). The symptom-based decision rule is intended to identify participants with PASC. PASC status for participants who do not meet the score threshold requires consideration of additional data inputs. B, Symptom frequencies among PASC-positive participants for symptoms contributing to the PASC score. Many other symptoms have a high frequency in PASC-positive participants (eTable 8 in Supplement 3). C, Distribution of the 10 overall Patient-Reported Outcomes Measurement Information System (PROMIS) responses among participants with a PASC score of zero and among participants within non-zero PASC score quintiles. PROMIS Global 10 provides an assessment of quality of life along 10 dimensions, each rated on a 5-point scale. Shading corresponds to the frequency within each column on a scale of 0% to 100%.
Conclusions and relevance
A symptom-based definition of post-acute sequelae of SARS-CoV-2 infection cases (PASC) was developed in a prospective cohort study. As a first step in providing a framework for further research, iterative refinement is needed that further incorporates other clinical characteristics to support actionable definitions of PASC.
Discussion
This study reported the first results from a prospective survey-based cohort of SARS-CoV-2-infected and uninfected adults with verification of patient-reported symptoms. A data-driven scoring framework was developed to classify PASC as a condition specific to SARS-CoV-2 infection. Based on this PASC score, 10% of participants who were first infected on or after December 1, 2021 and enrolled within 30 days of infection were classified as PASC positive at 6 months post-infection. . Increasing levels of PASC score were associated with progressively worse measures of well-being and functioning. Although only 12 symptoms contributed to the PASC score, other symptoms correlated with this subgroup are individually important, considering their potential adverse impact on health-related quality of life.
PASC positivity was more common and associated with more severe manifestation in participants infected in the pre-Omicron era . Although participants with prior infection may have been enrolled in the RECOVER adult cohort due to known PASC, several studies have reported an association between PASC and early pandemic variants. Among participants with a first infection during the Omicron era, the frequency of PASC was higher among those with recurrent infections, corroborating studies based on electronic health records. Although studies on the effect of vaccination are conflicting, these findings of modest reduction in PASC frequency among fully vaccinated participants align with recent systematic reviews.
This study found that long-term symptoms associated with SARS-CoV-2 infection spanned multiple organ systems . The diversity of symptoms may be related to persistent viral reservoirs, autoimmunity, or direct differential organ damage . The symptoms identified are consistent with those reported in studies evaluating the manifestations of PASC. However, by simultaneously considering the contributions of multiple self-reported symptoms, a PASC scoring algorithm was developed that provides a framework for diagnosing PASC.
Given the heterogeneity of PASC symptoms, it is important to determine whether PASC represents a unified condition or reflects a group of unique phenotypes. Recent evidence supports the presence of PASC phenotypes , although the characterization of these phenotypes is inconsistent and largely dependent on available data. Accurate phenotypic stratification has important implications for research into the pathophysiological processes underlying PASC and for the design of clinical trials.
This symptom-based definition of PASC represents a first step in identifying PASC cases and serves as a starting point for future research. Defining a classification rule for PASC requires an updated algorithm that incorporates symptoms and biological characteristics. Future analyzes should consider relationships between age, sex, race and ethnicity, social determinants of health, vaccination status after the index date, comorbidities, and pregnancy status during infection. PASC risk and the distribution of PASC subgroups.
















