Key points Is there an association between bariatric surgery and the incidence of obesity-related cancer and cancer-related mortality in patients with obesity? Findings In this retrospective cohort study of 30,318 patients (including 5,053 patients who underwent bariatric surgery and 25,265 matched patients in the nonsurgical control group), bariatric surgery was significantly associated with a lower risk of obesity-related cancer (hazard ratio, 0.68) and cancer-related mortality (hazard ratio, 0.52). Meaning Among adults with obesity, bariatric surgery compared with no surgery was associated with a significantly lower incidence of obesity-associated cancer and cancer-related mortality. |
Obesity increases the incidence and mortality of some types of cancer. With the prevalence of obesity increasing worldwide, the public health effects of obesity-associated cancer are considerable. It remains uncertain whether intentional weight loss can decrease this risk. Conducting randomized clinical trials with sufficient power and adequate follow-up to evaluate the effects of intentional weight loss on cancer incidence and mortality is extremely difficult. The incidence of cancer is relatively low and there is a long interval between the exposure (weight loss) and the outcome (development of cancer). Furthermore, many patients with obesity are unable to achieve substantial, sustained weight loss with lifestyle modifications alone, which would likely be necessary to significantly influence cancer risk.
Bariatric surgery is the most effective treatment currently available for obesity. Patients typically lose 20% to 35% of their body weight after surgery, which is often maintained for many years. 5 - 9 Some observational studies have reported an association between bariatric surgery and cancer risk reduction. Although they add important findings to the literature, they also leave the opportunity to answer additional questions. For example, reliable data are lacking on cancer-related mortality and on the risk of cancer after different surgical procedures, which clearly alter the anatomy.
This study was designed to investigate the relationship between contemporary bariatric procedures and the incidence of a large number of cancers and cancer-related mortality during long-term follow-up.
Importance
Obesity increases the incidence and mortality of some types of cancer, but it is not yet known whether intentional weight loss can reduce this risk.
Aim
To investigate whether bariatric surgery is associated with a lower risk of cancer and mortality in patients with obesity.
Design, environment and participants
In the SPLENDID (Surgical Procedures and Long-Term Effectiveness in Incidence and Death from Neoplastic Diseases) matched cohort study, adult patients with a body mass index of 35 or greater who underwent bariatric surgery in a US healthcare system .USA between 2004 and 2017 were included. Patients who underwent bariatric surgery were matched 1:5 with patients who did not undergo surgery for obesity, resulting in a total of 30,318 patients. Monitoring ended in February 2021.
Exhibitions
Bariatric surgery (n = 5,053), including Roux-en-Y gastric bypass and sleeve gastrectomy, versus nonsurgical care (n = 25,265).
Main results and measures
Multivariable Cox regression analysis estimated time to obesity-associated cancer incidence (a composite of 13 cancer types as the primary endpoint) and cancer-related mortality.
Results
The study included 30,318 patients (median age, 46 years; median body mass index, 45; 77% women and 73% white) with a median follow-up of 6.1 years (IQR, 3.8-8. 9 years). The mean between-group difference in body weight at 10 years was 24.8 kg (95% CI, 24.6-25.1 kg) or 19.2% (95% CI, 19.1%-19 .4%) greater weight loss in the bariatric surgery group.
During follow-up, 96 patients in the bariatric surgery group and 780 patients in the nonsurgical control group had an incident obesity-associated cancer (incidence rate of 3.0 events vs. 4.6 events, respectively, per 1000 person-years).
The 10-year cumulative incidence of the primary endpoint was 2.9% (95% CI, 2.2%-3.6%) in the bariatric surgery group and 4.9% (95% CI, 2.2%-3.6%) in the bariatric surgery group. %, 4.5%-5.3%) in the nonsurgical control group (absolute risk difference, 2.0% [95% CI, 1.2%-2.7%]; adjusted hazard ratio, 0.p = 0.002).
Cancer-related mortality occurred in 21 patients in the bariatric surgery group and 205 patients in the nonsurgical control group (incidence rate of 0.6 events vs. 1.2 events, respectively, per 1000 person-years) . The 10-year cumulative incidence of cancer-related mortality was 0.8% (95% CI, 0.4%-1.2%) in the bariatric surgery group and 1.4% (95% CI, 0.4%-1.2%) in the bariatric surgery group. 95%, 1.1%-1.6%) in the nonsurgical control group (absolute risk difference, 0.6% [95% CI, 0.1%-1.0%], adjusted hazard ratio , 0.52 [95% CI, 0.31-0.88], P= 0.01).
Figure : Weight loss and cumulative incidence of primary endpoint stratified by maximum weight loss quartile
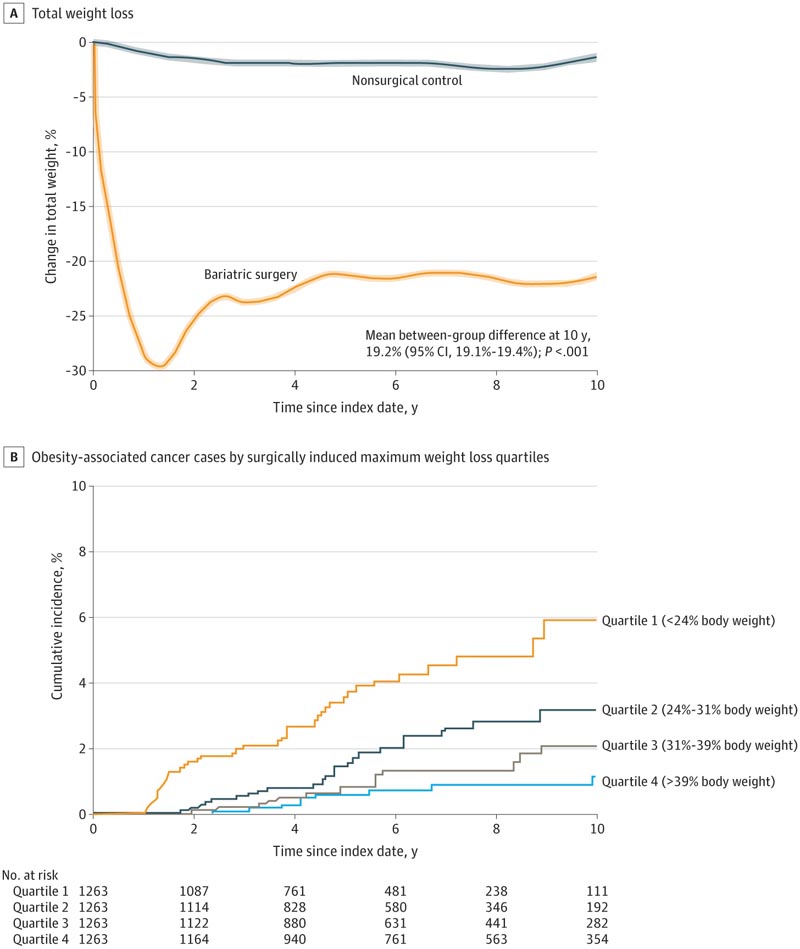
A, Data were smoothed and are mean trends for percent change in body weight from baseline in patients in the bariatric surgery group and the nonsurgical control group during follow-up. Shaded areas indicate 95% CIs. The mean difference between groups at 10 years from baseline was estimated from a flexible regression model with a restricted cubic spline of 4 knots for the time × treatment interaction. The median observation time was 5.9 years (IQR, 3.4-9.0 years) for patients in the bariatric surgery group and 6.3 years (IQR, 4.0-9.2 years) for patients in the bariatric surgery group. for patients in the non-surgical control group. B, Data are Kaplan-Meier estimates for the incidence of obesity-associated cancers by maximum (greatest) weight loss quartile in the bariatric surgery group ( P < .001 from log-rank test ). The findings suggest that weight loss in the bariatric surgery group was associated with a lower risk of incident cancer in a dose-dependent response.
Conclusions and relevance Among adults with obesity, bariatric surgery compared with no surgery was associated with a significantly lower incidence of obesity-associated cancer and cancer-related mortality. |
Reference : Association of Bariatric Surgery With Cancer Risk and Mortality in Adults With Obesity. Ali Aminian, Rickesha Wilson, Abbas Al-Kurd, et al. JAMA. 2022;327(24):2423-2433. doi:10.1001/jama.2022.9009
















