Aim
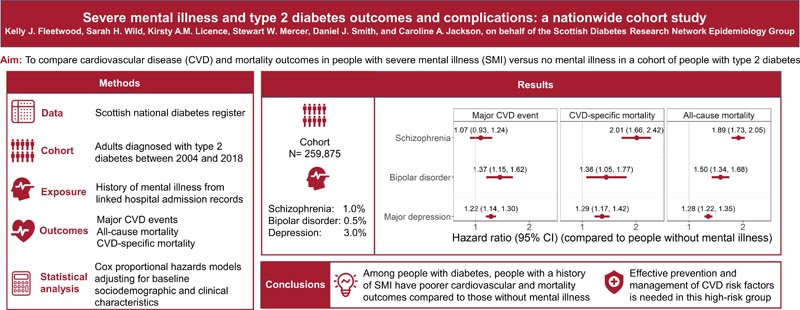
To compare cardiovascular and mortality outcomes in people with serious mental illness (SMI) versus no mental illness in a national cohort study of people with type 2 diabetes.
Methodology
We included adults diagnosed with type 2 diabetes between 2004 and 2018 from the Scottish national diabetes register, determining history of mental illness from linked psychiatric and general hospital admission records.
We identified major cardiovascular disease (CVD) events, all-cause mortality, and CVD-specific mortality through record linkage.
Using Cox regression, we estimated hazard ratios (HRs) for associations between SMI and outcomes, adjusting for baseline sociodemographic and clinical characteristics, including history of CVD, comorbidity, hypertension, high cholesterol, HbA 1c, BMI , alcohol use disorder and smoking.
Results
Among 259,875 people with type 2 diabetes, 1.0%, 0.5%, and 3.0% had schizophrenia, bipolar disorder, and major depression, respectively.
After adjusting for sociodemographic characteristics, the risk of major CVD events was higher in people with schizophrenia (HR 1.22, 95% CI 1.06–1.41), bipolar disorder (HR 1.58, 95% CI 1, 33–1.87) and major depression (HR 1.59). , 95% CI: 1.49–1.70) compared with people without a history of mental illness.
Severe mental illness (SMI) was also associated with an approximately twofold increased risk of CVD-specific and all-cause mortality.
All associations were attenuated after further adjustment for clinical characteristics.
Conclusions
|
















